Ovulation Disorders
Overview
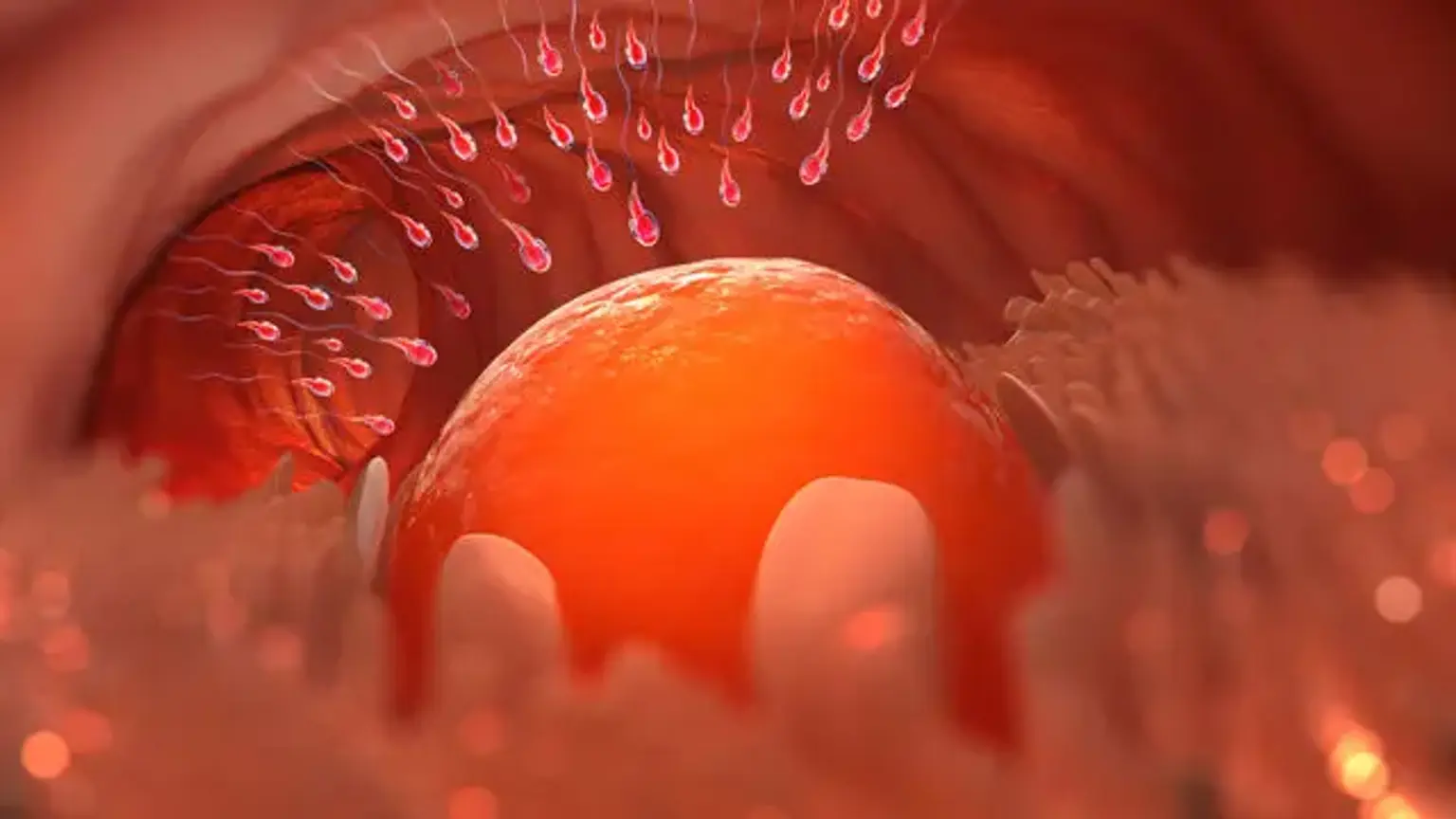
Ovarian continuity may be thought of as a process that happens throughout a woman's life and begins with fertilization during intrauterine life. Women begin their reproductive years with roughly 500,000 follicles holding oocytes, of which only about 500 will be released during ovulation. Ovulation has long been regarded as a reproductive event; nevertheless, new data supports the relevance of ovulation as a health indicator.
The use of biomarkers that assist women in recognizing ovulation allows them to determine their health state. This information assists medical healthcare practitioners in the prevention, diagnosis, and treatment of endocrine problems, gynecological abnormalities, autoimmune, genetic, and neoplastic illnesses, as well as pregnancy-related difficulties.
Understanding the ovarian continuum and using biomarkers to detect ovulation should be seen as a strong tool for both women and medical professionals.