Pancreatitis
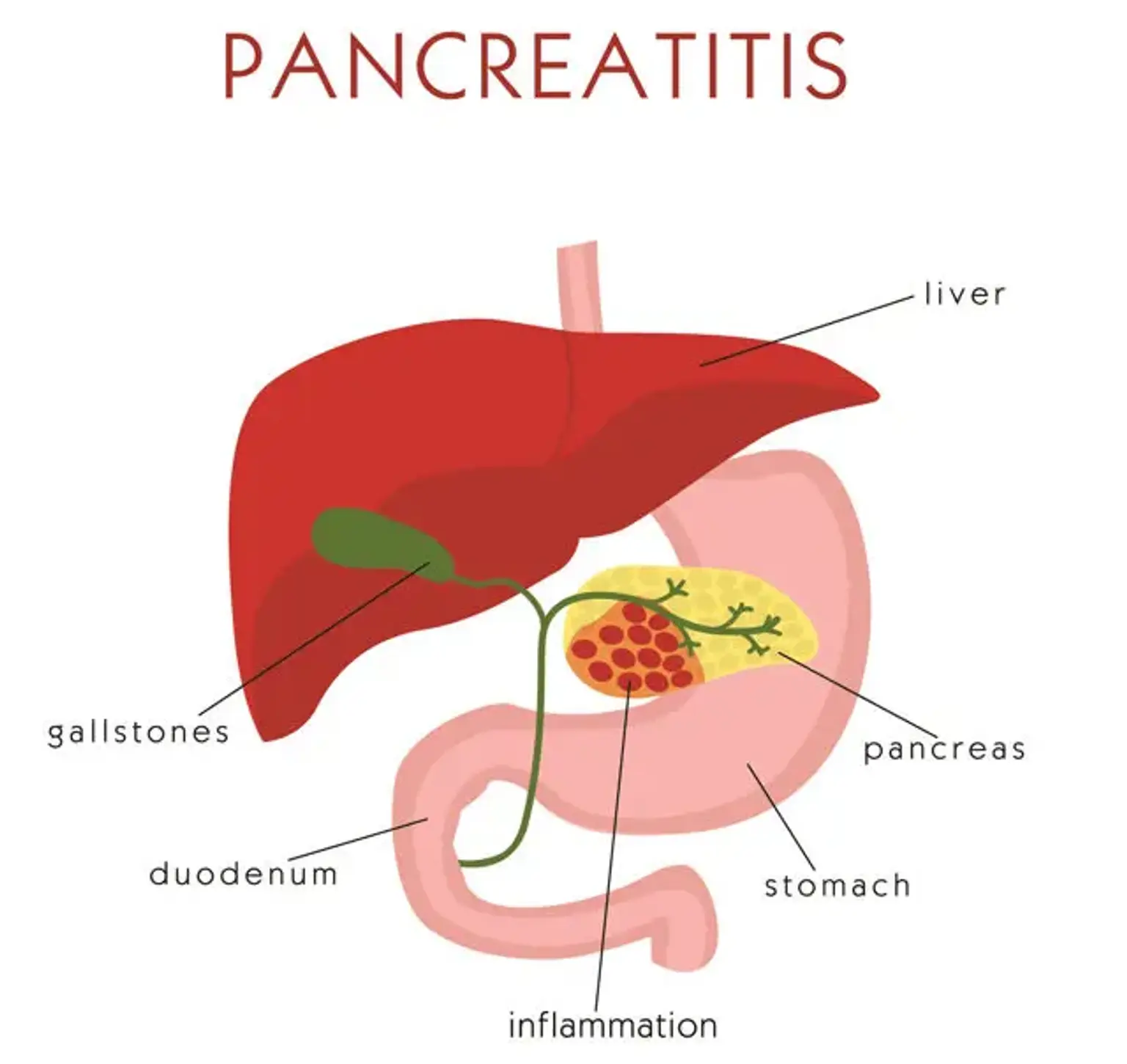
Pancreatitis is a condition characterized by inflammation of the pancreas. The pancreas is the long flattened gland located behind the stomach near the small intestines. It plays a vital role in producing enzymes that facilitate digestion. It also releases hormones that regulate how the body processes glucose or sugar.
Damage can occur when the digestive enzymes start to work even before the pancreas generates them. Among other causes, the most common triggers of pancreatitis involve consumption of alcohol and gallstones. It can either emerge or disappear within a short period even without treatment or can be severe with fatal complications.