Parathyroid Disease
Overview of Parathyroid Disease
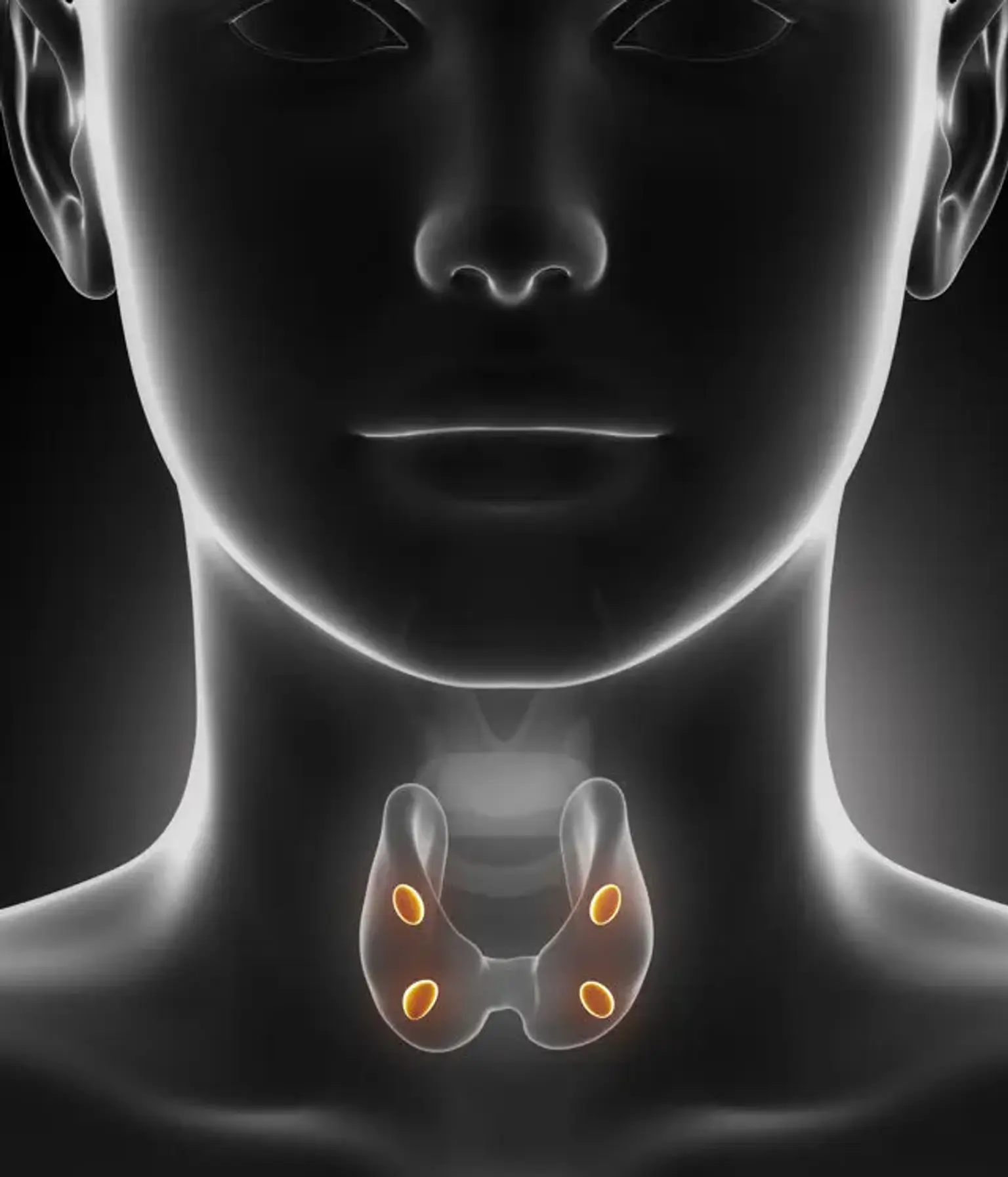
The parathyroid glands are located in the neck, right beneath the thyroid glands. The parathyroid glands (light pink) secrete parathyroid hormone, which raises calcium levels in the blood.
The most frequent symptom of a parathyroid gland disorder is an increase in blood calcium levels. Primary hyperparathyroidism, the most prevalent cause of hypercalcemia in outpatients, is generally asymptomatic or may be associated with bone disease, nephrolithiasis, or neuromuscular symptoms. Chronic kidney disease patients may develop secondary hyperparathyroidism, resulting in chronic kidney disease-mineral and bone conditions.
Hypoparathyroidism is most commonly caused by neck surgery; however, it can also be caused by autoimmune destruction of the glands and other less prevalent issues. A history and physical examination are performed on individuals with abnormal blood calcium levels, as is a repeat test of serum calcium levels, as well as measurements of creatinine, magnesium, vitamin D, and parathyroid hormone levels.