Pediatric flexible bronchoscopy
Overview
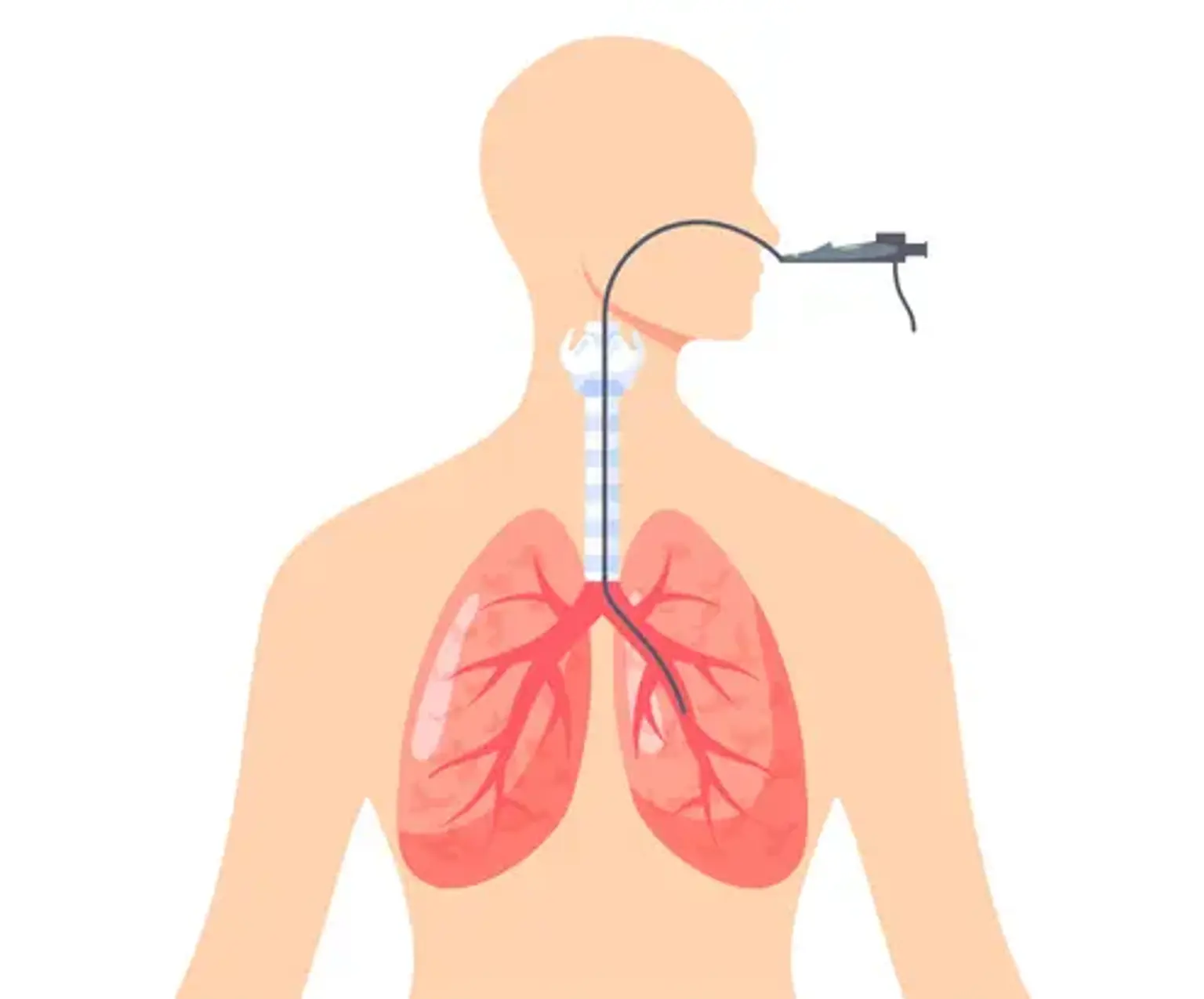
Flexible bronchoscopy (FB) is a critical procedure for assessing the pediatric airway, voice cords, trachea, bronchi, and bronchioles. A flexible bronchoscope is introduced via the nose or mouth into the lungs while your kid is sedated. The bronchoscope is a specialized equipment equipped with a small camera that allows the pediatric pulmonologist to observe the anatomy through the scope or on a video display.
Other procedures, such as Bronchoalveolar lavage (cleaning), transbronchial biopsy (removing tiny pieces of tissue), endobronchial ultrasonography, electrocautery, or laser therapies, are possible using the bronchoscope.
Bronchoscopy, in general, assists in the visualization of airway anatomy (e.g., agenesis), the assessment of airway dynamics (e.g., malacia), the localization and treatment of obstructions (e.g., mucus plugs), the collection of fluid samples (i.e., bronchoalveolar lavage (BAL), and brushing/biopsy for microbiology and histopathology. Suctioning, re-inflation, therapeutic wash out, medicine delivery, and counseling for difficult intubation are other therapeutic reasons.