Percutaneous Coronary Intervention
Coronary artery disease, or CAD, is a type of heart disease that can be managed with drugs as well as dietary and lifestyle modifications. In the event that your situation worsens, your doctor may recommend percutaneous coronary intervention, or PCI, to treat your heart arteries.
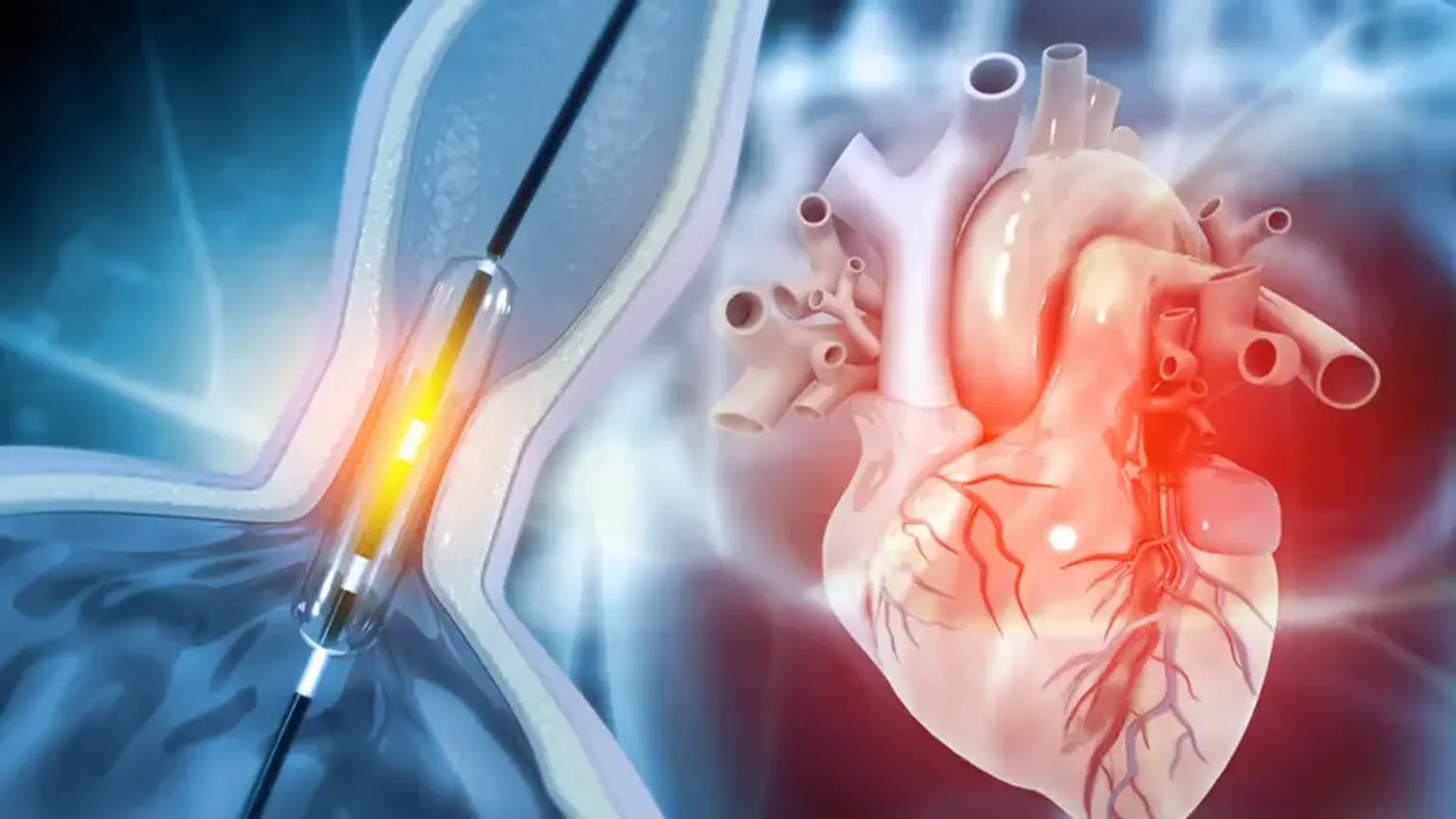
Procedures to open occluded coronary arteries, blood vessels that give oxygen to your heart muscles via blood, are referred to as percutaneous coronary intervention.
Plaque, which is made up of fatty materials like cholesterol, can build up in these arteries, leaving them stiff and narrow, restricting blood flow and leading to coronary artery disease (CAD).
Heart damage, chest pain, difficulty breathing, fatigue, and an increased risk of heart attack can all be symptoms of poor blood flow to the heart. With time, your heart can deteriorate, which can result in heart failure.