Pituitary tumors
Overview
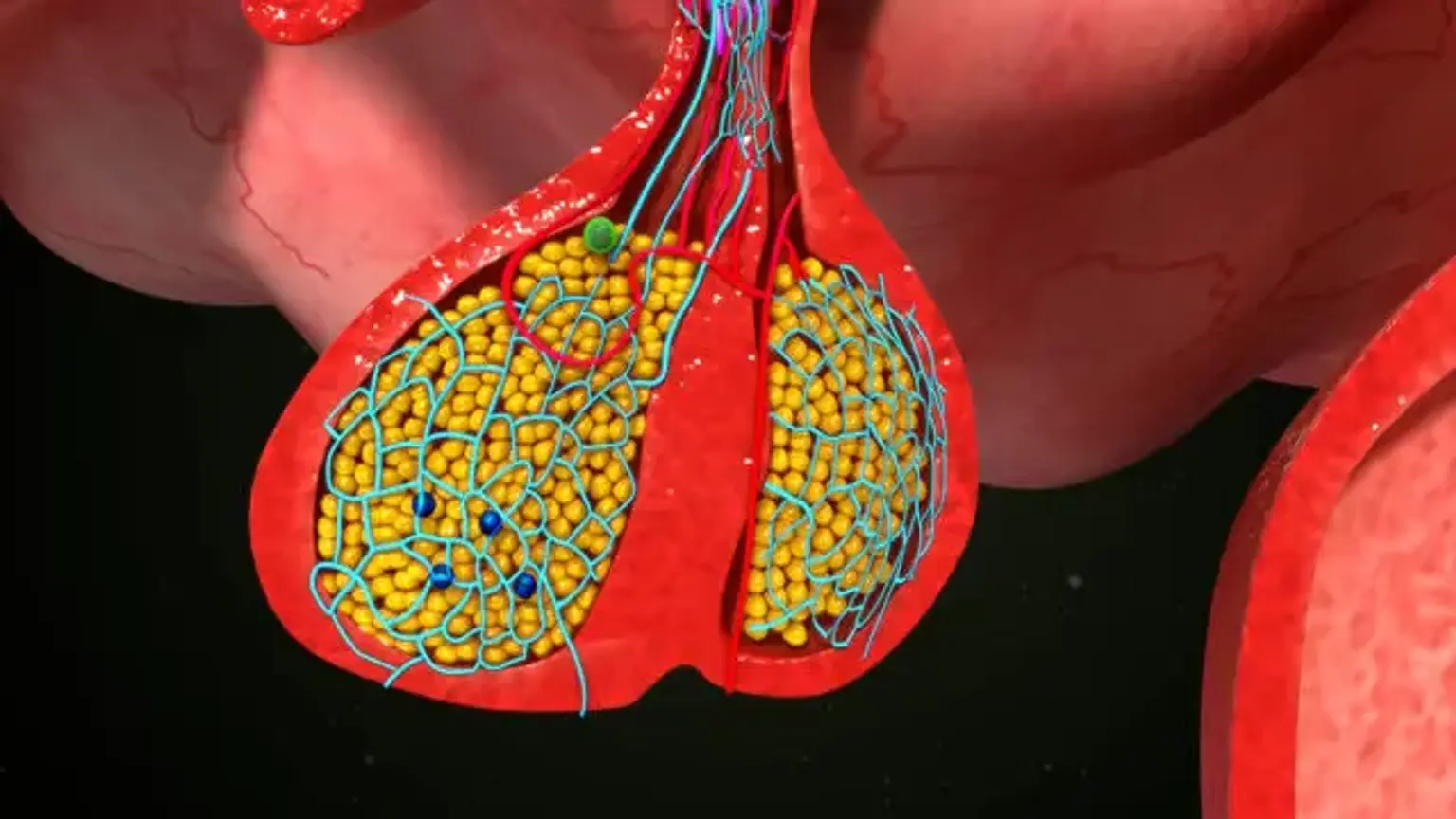
Different hormone gene products are expressed by anterior pituitary cell types. ACTH, GH, PRL, TSH, FSH, and LH are among them. Pituitary adenomas are distinguished by both excessive proliferation of one of these differentiated cell types and abnormally high levels of specific hormone hypersecretion. In tightly regulated regulatory loops, the six pituitary trophic hormones govern respective target hormone synthesis and endocrine gland function. Adenoma hypersecretion is generally caused by a malfunction in hormone production or secretion.
Each of these cell-specific adenomas is linked with a benign sellar mass as well as a distinct clinical condition caused by the hypersecretion of the hormone. Thus, lactotroph adenomas cause hyperprolactinemia with hypogonadal characteristics and galactorrhea.
Corticotroph adenomas hypersecrete ACTH, resulting in hypercortisolism symptoms such as central obesity, hypertension, hyperglycemia, infections, and psychological disorders. Somatotroph adenomas oversecrete GH, resulting in acromegaly symptoms such as acral alterations, arthritis, hypertension, headache, soft tissue edema, and hyperglycemia. Thyrotroph adenomas that produce excessive TSH are exceedingly uncommon and may be linked with moderate hyperthyroidism and goiter.