Prostatic hyperplasia
Overview
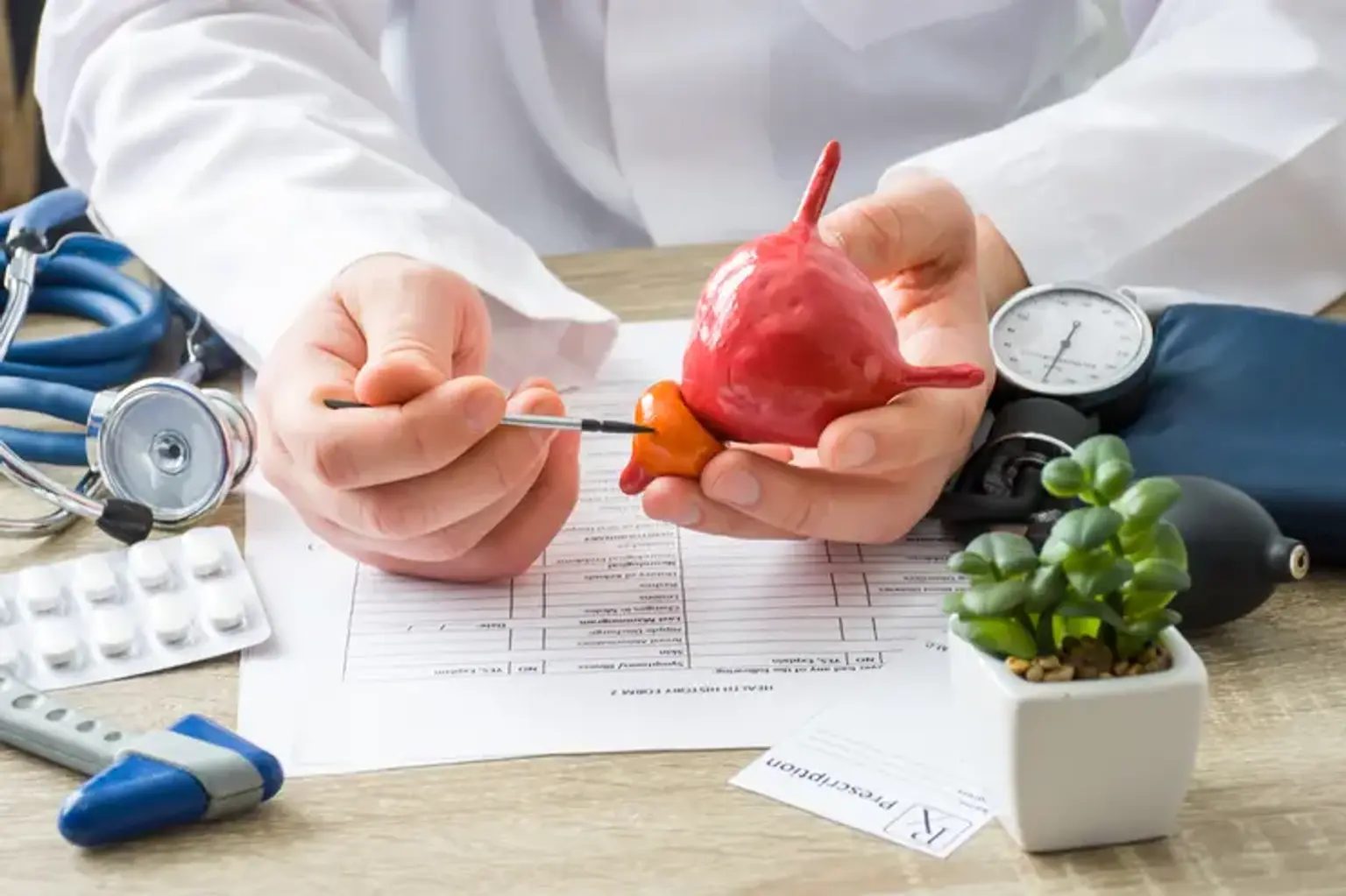
The prostate gland is a walnut-shaped gland in the male reproductive system. The prostate's primary role is to produce a fluid that enters sperm. Prostate fluid is required for male fertility. At the bladder's neck, the gland surrounds the urethra. The bladder neck is the junction of the urethra and the bladder. The lower urinary tract includes the bladder and urethra. The prostate consists of two or more lobes or parts surrounded by an outer layer of tissue and is located in front of the rectum, right below the bladder. The urethra is the tube that transports urine from the bladder to the exterior of the body. In men, the urethra also transports sperm to the penis.
The prostate is not required for life, but it is necessary for reproduction. Healthy sperm has the ideal consistency and habitat for transit and survival, as well as fertilization. Semen contains enzymes such as PSA (which is frequently examined as part of prostate cancer screening) as well as other components produced by the seminal vesicles and prostate such as zinc, citrate, and fructose (that actually gives sperm energy to make the journey to the egg). Semen also includes antibacterial and antiviral chemicals that may protect the urinary system and sperm from bacteria and other diseases.
The prostate is separated into anatomic zones or areas. The vast majority of prostate cancers begin in the peripheral zone (the rear of the prostate), near the rectum. That is why, in addition to the PSA blood test, a digital rectal exam (DRE), in which a clinician checks the prostate by inserting a gloved finger into the rectum, is a popular and beneficial screening test.