Psoriasis Arthritis
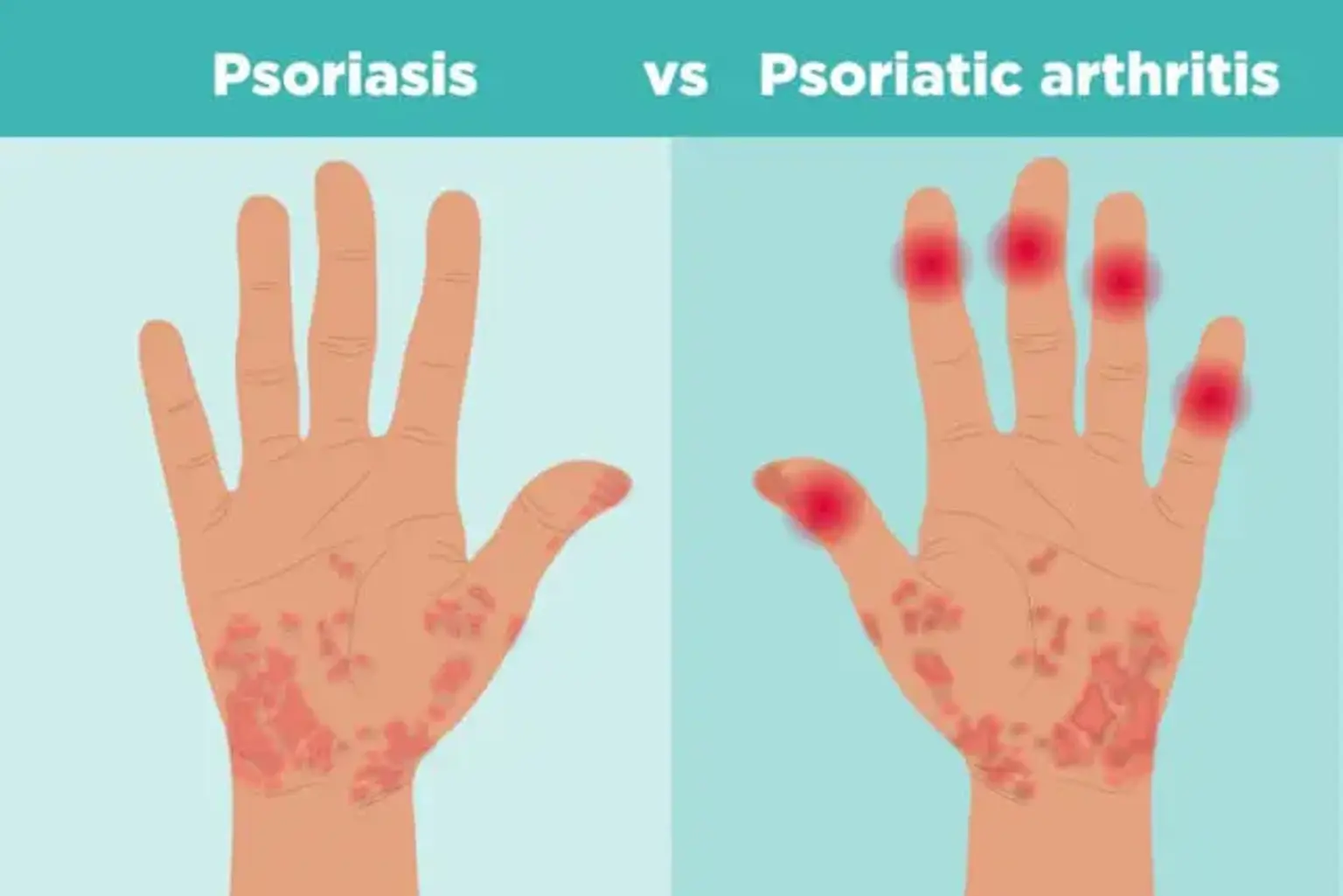
Psoriasis arthritis is a type of arthritis characterized by swelling, joint pain, and stiffness. It can affect people with psoriasis, a disorder that causes scaly and itchy red patches on the skin or scalp. Many individuals get psoriasis first before they are later detected with psoriasis arthritis. However, the joint issues may at times develop before the appearance of the skin patches.
Psoriasis arthritis can occur in any area of the body, such as the spine and fingertips. They also range from fairly moderate to chronic. In both cases of psoriasis and psoriasis arthritis, the condition flares tend to alternate with remission periods.