Pulmonary Artery Catheterisation
Since Swan and Ganz and associates introduced pulmonary artery catheterization, there has been a lot of debate about its value. However, a study published by Connors and colleagues compared the consequences of critically ill patients treated with or without a pulmonary artery catheterization within the first 24 hours after admission to an intensive care unit and found a link between pulmonary artery catheterization and a steadily increasing relative risk of hospital mortality and resource utilization. This research renewed the debate and prompted physicians to reconsider the pulmonary artery catheterization efficacy and safety. Many studies demonstrate that pulmonary artery catheterization has almost no value or risk, while others demonstrate that it reduces death. Despite the controversies, doctors continue to utilize pulmonary artery catheterization in critically ill patients despite the lack of documented justifications.
Several hemodynamic measures are obtained using pulmonary artery catheterization. Heart rate, rhythms, cardiac output, pulmonary artery pressures, right atrial pressure (central venous pressure), pulmonary arterial occlusion pressure (wedge pressure), and mixed venous oxygen saturation are among the parameters that can be directly monitored. Many additional data, such as mean arterial pressure, body surface area, stroke volume, systemic and pulmonary vascular resistance, ventricular stroke workload, and oxygen supply and demand, can also be estimated using these variables.
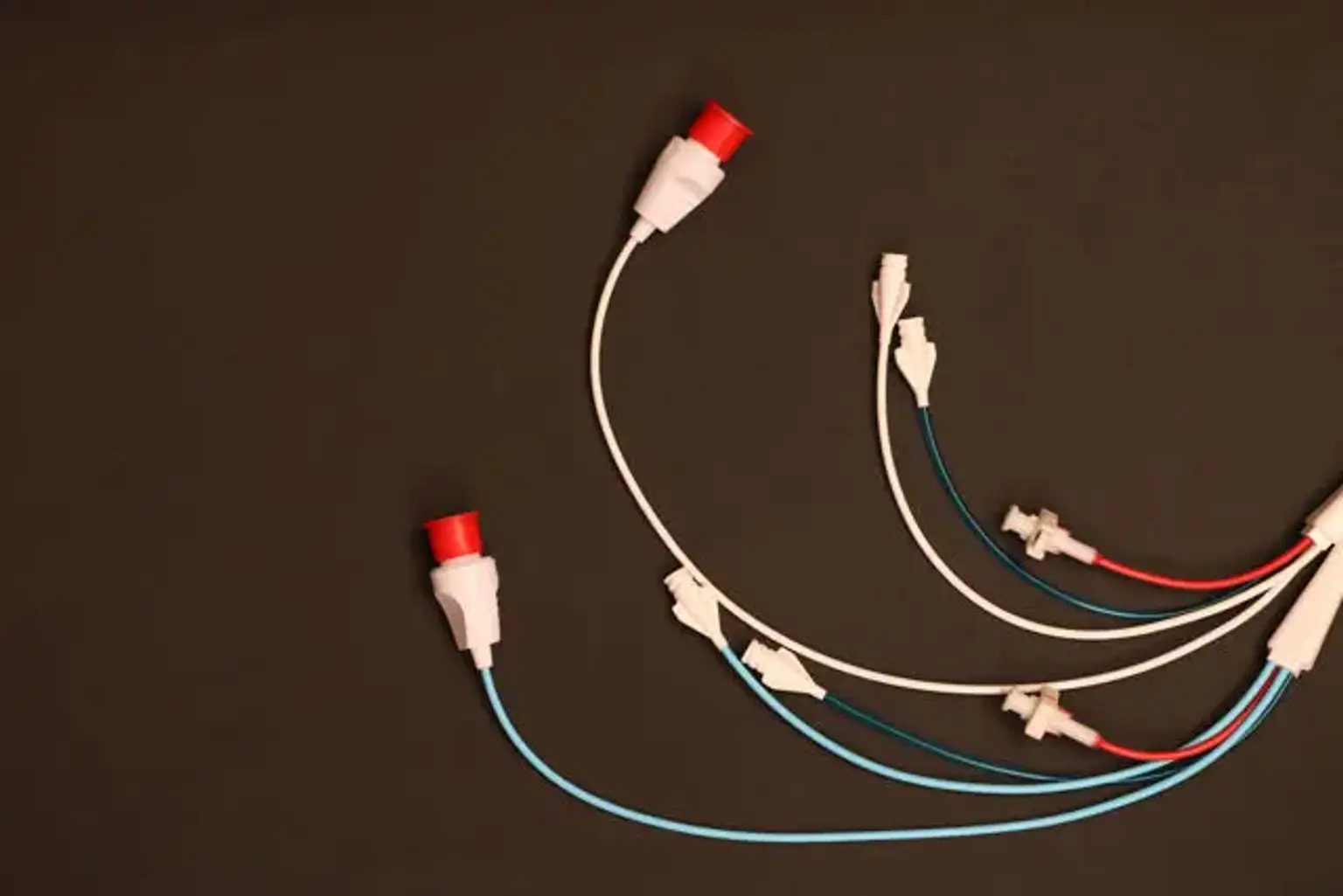
A pulmonary artery catheter was originally intended to treat acute myocardial infarction, but it has since been used to treat a wide range of critical illnesses and surgical interventions.