Radiofrequency ablation
Overview
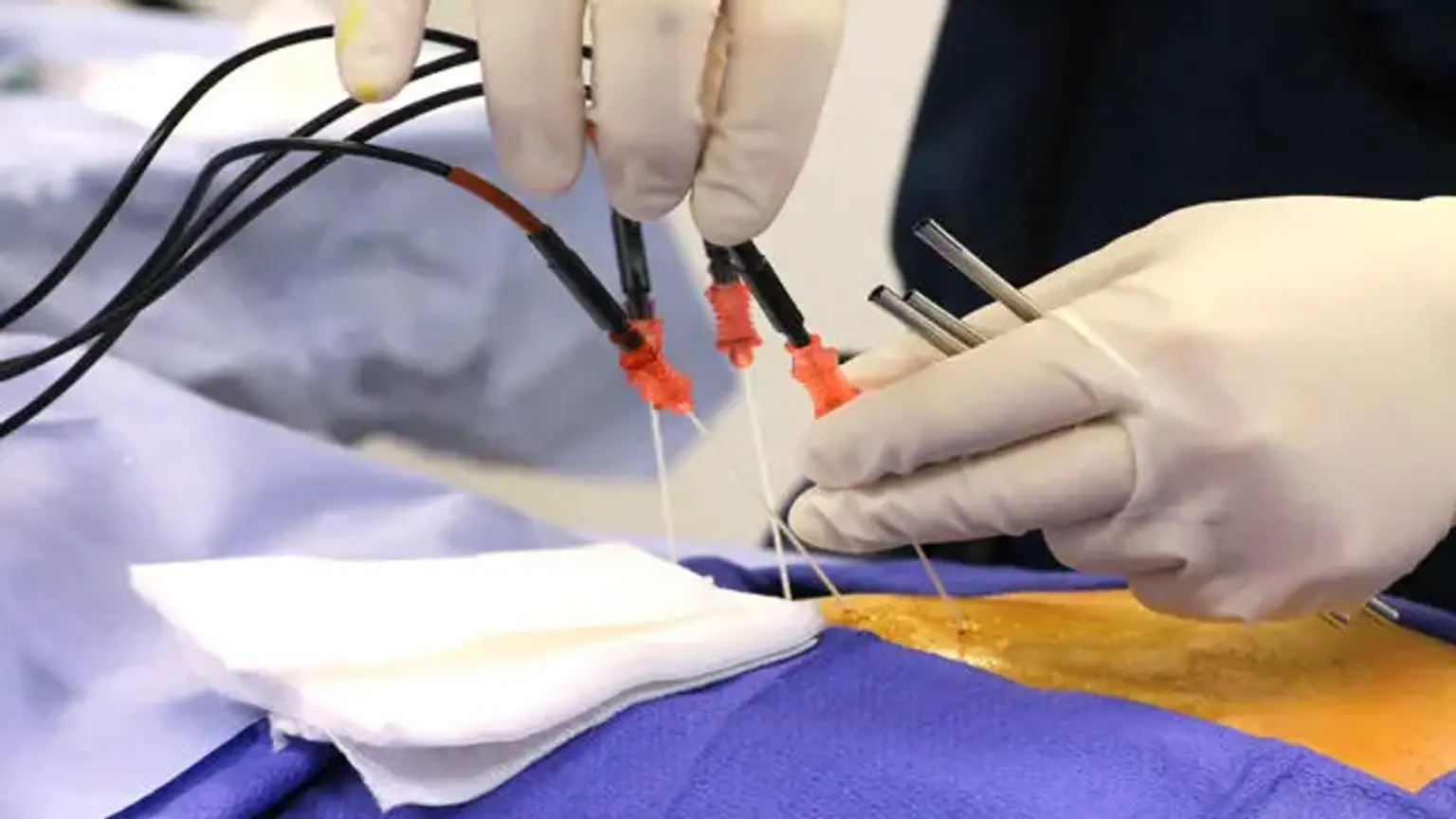
Radiofrequency ablation involves the use of an electric current to burn up a tiny region of nerve tissue in order to prevent it from delivering pain signals. It can give long-term relief for patients suffering from chronic pain, particularly in the lower back, neck, and arthritic joints.
The use of radiofrequency ablation for chronic pain is based on the assumption that passing radiofrequency currents near nociceptive pathways may disrupt pain signals. The heat energy linked with radiofrequency ablation causes tissue damage, with the nerves responsible for transmitting and/or modifying pain sensations being targeted.