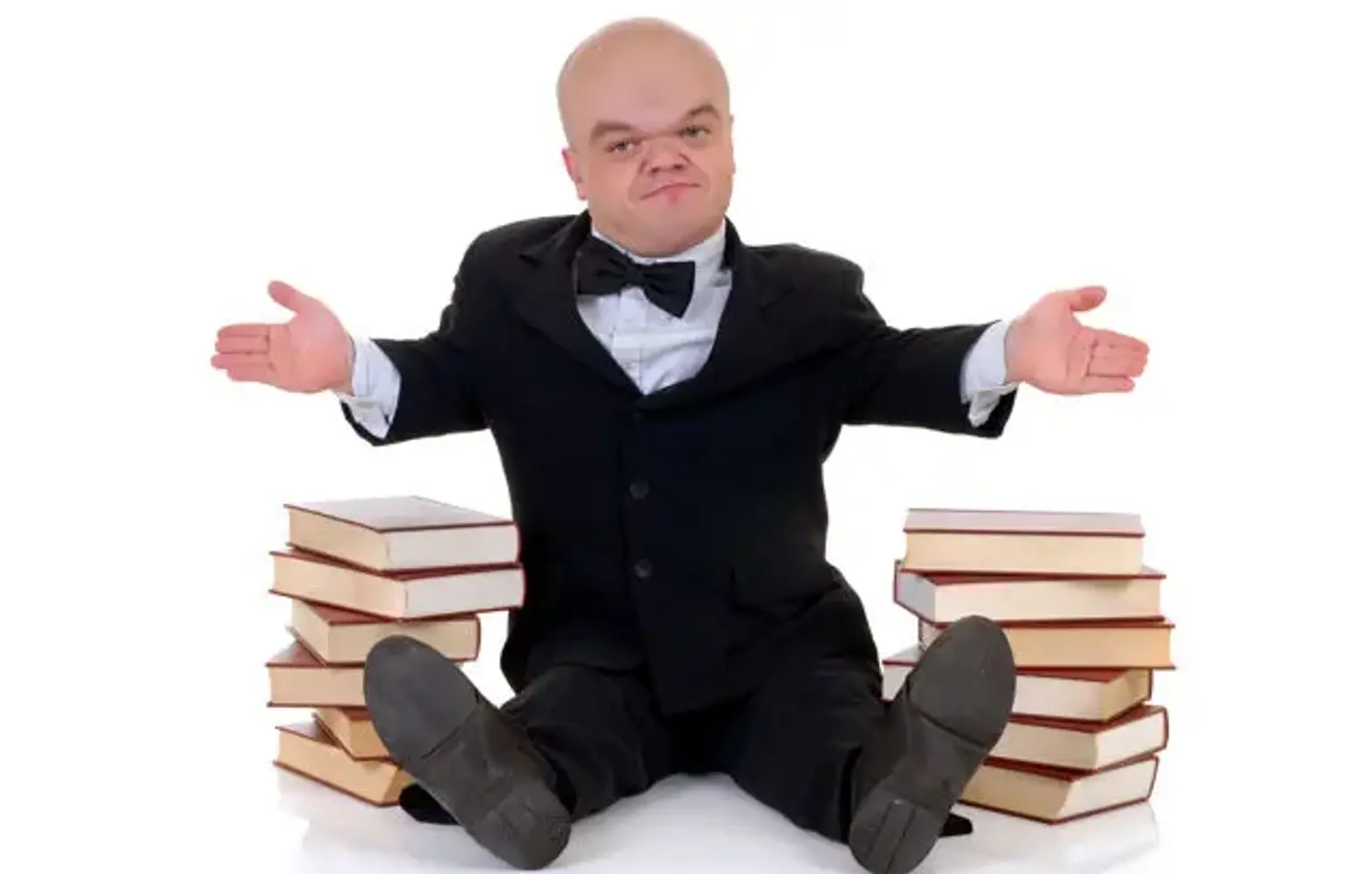
Skeletal dysplasia
Overview
Skeletal dysplasias are a collection of over 450 heritable bone abnormalities. They frequently show with disproportion, radiographic abnormalities, and, on rare occasions, other organ system abnormalities throughout the newborn period. It is critical to get a specific diagnosis to aid in management, family recurrence, and identifying those illnesses that are highly related with mortality in order to provide better therapeutic care.
Long-term management of these illnesses is dependent on an awareness of the associated skeletal system anomalies, and these children benefit most from a team approach to health care surveillance.