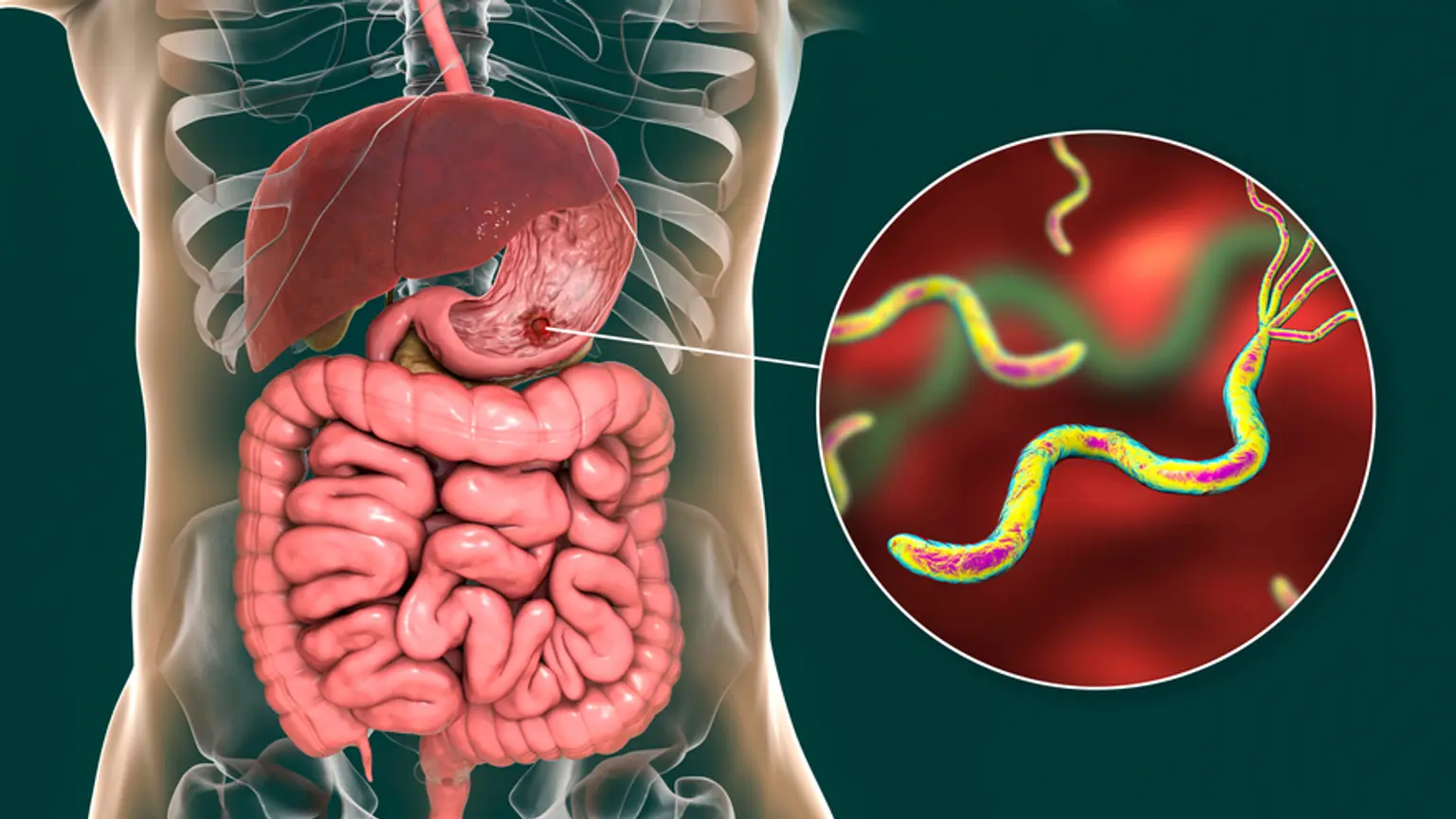
Stomach and duodenal diseases
Overview
If you have symptoms like heartburn, nausea, vomiting, stomach pains, or difficulty swallowing, you may have an upper GI (gastrointestinal) tract problem. If you consistently have these symptoms, it may be time to seek the advice of a gastroenterologist for additional examination in order to successfully treat the underlying disease.