Stroke
Overview
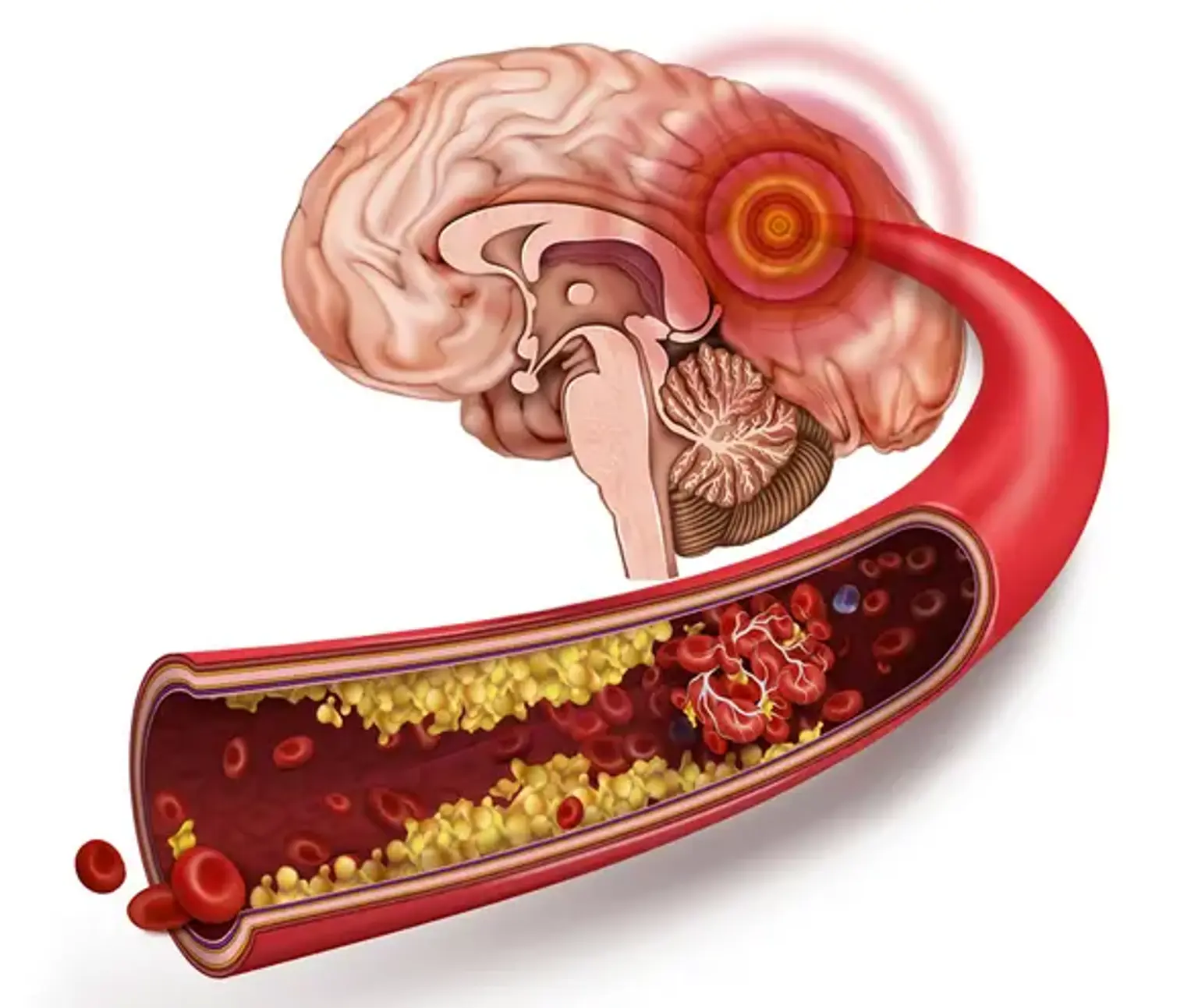
Cerebrovascular accidents, often known as strokes, are common across patient populations and can be a major cause of morbidity and mortality. Strokes are classified as either ischemic, hemorrhagic, or subarachnoid. Understanding your stroke can help you understand how your brain operates.