Surgical Treatment of Epilepsy
Overview
With a global frequency of roughly 0.8 percent, epilepsy is one of the most frequent neurologic illnesses. Antiepileptic medications (AEDs) constitute the basis of therapy in underdeveloped nations. Despite the fact that the majority of patients with epilepsy will have excellent seizure control with medication, around 30% will fail anti-epileptic medicines. Recurrent seizures raise mortality and injury risks in those with medically intractable epilepsy, and the episodes themselves are socially burdensome.
Fortunately, for many patients suffering from intractable epilepsy, epilepsy can be cured or seizures can be managed more effectively with surgical therapy.
Epilepsy surgery
Approximately one-third of epilepsy patients suffer seizures that are uncontrollable with medication. This has serious repercussions, such as disruptions in school and employment, loss of independence and social isolation, and an increased risk of injury, despair, and suicide. Patients with uncontrolled epilepsy have a much higher long-term mortality rate, with the most prevalent cause being sudden unexpected death in epilepsy. Furthermore, uncontrolled temporal lobe epilepsy is linked to gradually increasing cortical atrophy and cognitive decline.
Localization of the seizure focus, followed by surgical excision, offers the best chance of curing epilepsy, and a greater knowledge of the neuro-anatomy and physiology of epilepsy increases our capacity to identify the epileptic network and successfully treat epilepsy. Minimal access surgical methods, which result in faster recovery after surgery, less pain, and happier patients, are an essential advancement that has improved patient care.
Furthermore, even those who do not have a chance of curing their epilepsy, new and coming technologies promise to lower seizure frequency and intensity, enhancing quality of life and reducing injuries and mortality caused by intractable epilepsy.
Relevant Anatomy
The cerebrum, brainstem, and cerebellum are the three major structural divisions of the brain. The brainstem is located at the base of the brain and runs from the upper cervical spinal cord to the diencephalon of the cerebrum. The brainstem is split into three sections: the medulla, pons, and midbrain. The cerebellum is located posterior to the brainstem.
The cerebrum is the brain's biggest component. It is separated into two halves: right and left. The longitudinal cerebral fissure separates the left and right cerebral hemispheres. The corpus callosum is the main link between the two hemispheres. Each hemisphere of the cortex is split into four lobes: frontal, temporal, parietal, and occipital. The lateral sulcus distinguishes the frontal lobe from the temporal lobe.
The central sulcus distinguishes the frontal lobe from the parietal lobe (Rolandic fissure). The parieto-occipital fissure, evident on the hemisphere's medial side, separates the parietal and occipital lobes. The insula is a cortical surface located within the lateral sulcus.
The frontal lobe is further subdivided into superior, middle, and inferior frontal gyri, which are separated by superior and inferior frontal sulci. The temporal lobe is similarly split into superior, middle, and inferior temporal gyri, which are separated by superior and inferior temporal sulci.
The superior temporal sulcus is topped by the angular gyrus inside the parietal lobe. The supramarginal gyrus caps the lateral sulcus just above this. The inferior temporal sulcus is capped by the lateral occipital gyrus, which is located just below the angular gyrus.
Reasons for considering surgical intervention
Although there are dangers associated with intracranial surgery, these risks do not outweigh the hazards of uncontrolled seizures. Seizures cause the following morbidity and mortality:
- Accidental injury
- Cognitive decline
- Sudden unexplained death in epilepsy (SUDEP)
- Psychological, social, and vocational impairment
Fractures, burns, tooth injuries, lacerations, and head traumas are all prevalent types of accidental injuries. Patients with certain epilepsy syndromes who have recurring convulsive seizures or periods of status epilepticus have been shown to have cognitive impairment and memory loss over time.
Patients with nonconvulsive and convulsive seizures had considerably higher mortality rates than age-matched controls. SUDEP can occur at a rate of one fatality per 500 patients per year in people with poorly managed epilepsy. Poorly managed seizures and low serum antiepileptic medication (AED) levels are risk factors.
Depression and anxiety are quite frequent among people suffering from medically resistant epilepsy. Intractable epilepsy prohibits people from driving and lowers fertility and marriage rates. Inability to find work or, if employed, underemployment are examples of vocational problems.
The aforementioned facts clearly indicate that for certain types of epilepsy, ongoing medical therapy following failure to control seizures with vigorous trials of AEDs is not ideal management.
In several retrospective trials and two prospective, randomized, controlled trials for a well-defined syndrome with a known favorable surgical outcome (ie, mesial temporal lobe epilepsy), the efficacy of surgery significantly outperforms that of continued AED treatment, and the morbidity and mortality associated with surgical treatment are lower than those associated with the disorder.
Criteria for surgical intervention
A candidate for epilepsy surgery must have failed to achieve satisfactory seizure control after a sufficient number of AED trials and must have a reasonable likelihood of benefitting from surgery. The following practice guidelines have been suggested by the American Academy of Neurology, the American Association of Neurological Surgeons, and the American Epilepsy Society:
- Patients with debilitating complex partial seizures, with or without secondary generalized seizures, who have failed acceptable trials of first-line AEDs should be referred to an epilepsy surgery center, even if criteria for medication treatment failure have not been definitively defined (level A)
- Patients referred to an epilepsy center for the reasons indicated above who satisfy established criteria for anteromedial temporal resection (AMTR) and who are willing to accept the risks and advantages of this technique over continued medication should be given surgical treatment.
Preoperative assessment
Classification and Preoperative Diagnosis of Epilepsy
Following a categorization of the patient's seizure types and particular epilepsy syndrome, a preoperative diagnosis is produced. The International League Against Epileptic (ILAE) recognizes 10 categories of recurring seizures and 40 types of epilepsy disorders. Both categorization approaches assume that seizures and epilepsies naturally fall into two primary groups depending on the location of seizure start in the brain:
- Partial (focal, localization-related) and
- Generalized.
The seizure diagnosis is determined by the patient's signs and symptoms (semiology) as well as the EEG pattern obtained during ictal onset. This procedure begins with meticulously documenting the past. A complicated partial seizure, for example, is likely to begin with a blank look and halt of motion and advance to the formation of automatisms.
A tentative diagnosis based on the background may sufficient for first AED therapy. Even in the best of conditions, a diagnosis based purely on history may be wrong. When surgical therapy for intractable epilepsy is being considered, the most accurate technique to determine the epileptic syndrome diagnosis and brain region of seizure origin is to employ long-term video-EEG (VEEG) monitoring.
The following is a simplification of the international classification of epileptic seizures:
- Partial seizures (seizures that begin locally) - These include:
- Simple partial seizures (consciousness not impaired),
- Complex partial seizures (consciousness impaired) and
- Partial seizures that secondarily progress to generalized tonic-clonic seizures.
- Generalized seizures (seizures that arise diffusely) - These include absence seizures, atypical absence seizures, clonic seizures, tonic seizures, tonic-clonic seizures, myoclonic seizures, and atonic seizures.
- Unclassified seizures
Structural and Metabolic Brain Imaging
Because seizures can be caused by cortical lesions or abnormalities, neuroimaging can frequently assist detect and pinpoint the source of the damage and, as a result, the location of seizure start. The following imaging modalities are available:
- Skull radiography
- Computed tomography (CT) scanning
- MRI
- PET
- Single-photon emission tomography (SPECT)
- Magnetoencephalography/magnetic source imaging (MEG/MSI)
In this context, standard skull films are of limited use. Because MRI produces better pictures, it has essentially supplanted routine CT scanning. The only exception to this rule is that CT scanning detects intraparenchymal calcium and acute bleeding better than MRI; this may be useful in differentiating specific types of malignancies or central nervous system (CNS) diseases (eg, tuberous sclerosis).
The finest structural imaging examination is without a doubt brain MRI. A comprehensive brain MRI examination with particular thin-cut coronal magnified images perpendicular to the axis of the temporal horn should be included in every surgical evaluation. These images may show mesial temporal sclerosis.
PET scanning, as opposed to MRI or CT scanning, displays brain glucose metabolism rather than structure. An interictal scan often reveals hypometabolism in the region of the epileptic focus; if obtained during a seizure, the normal finding is hypermetabolism from the focus.
Invasive Video-EEG Monitoring
When noninvasive testing indicates a resectable epileptic focus with some ambiguity, this procedure is used. Invasive video-EEG can also identify the breadth of a neocortical epileptogenic zone and its link to regions of eloquent functioning cortex more clearly. Subdurally implanted arrays of disk electrodes embedded in sheets or strips of silastic are commonly used.
Depth electrodes can also be placed into the brain, usually to record from deeper areas, however some centers employ them for cortical recordings as well. Over many days, the patient's room is monitored to locate typical seizures.
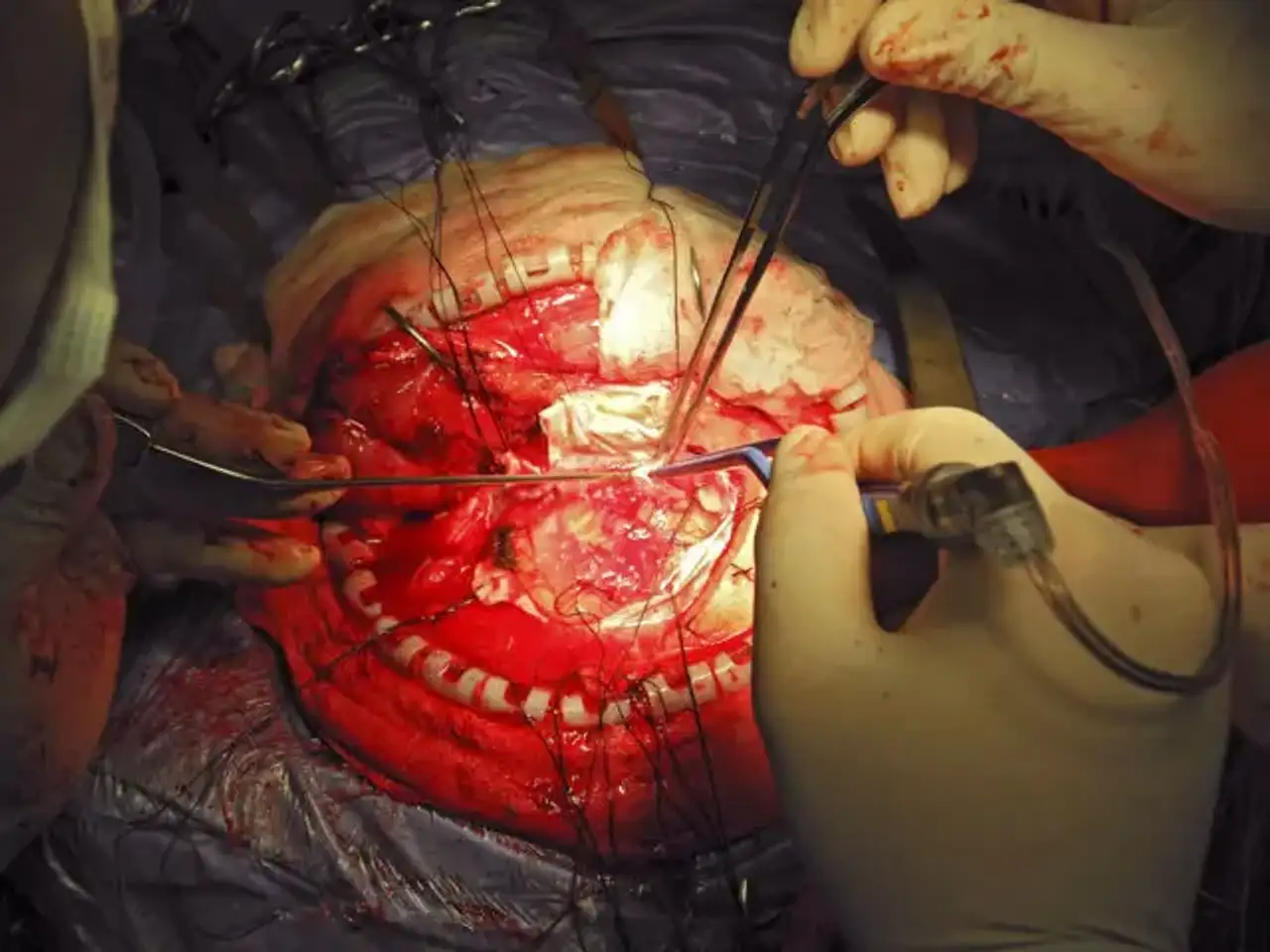
Surgical technique
The surgical strategy may be either definitive or palliative, as follows:
- Definitive – The goal is to eliminate all seizures, or at least reduce them by 70-90 percent; in general, these operations physically remove seizure-producing cortex from the brain.
- Palliative – The goal is to reduce seizure frequency (seizure independence is uncommon); these techniques often impair pathways involved in seizure formation and propagation or seek to interrupt seizures using electrical stimulation.
The following 4 procedures may be considered for the surgical treatment of epilepsy:
Anteromedial temporal resection (AMTR)
This is the most commonly performed procedure, with the clearest indications and best results
Indications for AMTR include the following:
- Complex partial seizures with semiology typical of mesial temporal lobe epilepsy
- Magnetic resonance imaging (MRI) evidence of unilateral hippocampal atrophy and increased T2-weighted signal (at some centers, volumetric measurements of the hippocampus are routinely obtained)
- Unilateral temporal lobe hypometabolism on positron emission tomography (PET) scans if MRI findings are nonlesional in nature
- EEG confirmation that seizures begin over the temporal area ipsilateral to the hippocampal atrophy or PET scan evidence of hypometabolism
Although AMTR has now been found to be more beneficial than continuous medication for mesial temporal lobe epilepsy, trials to far have included individuals who have had epilepsy that has been resistant to medical therapy for an extended length of time. The majority of patients who are eventually referred for AMTR have experienced epilepsy for about 20 years.
However, because ongoing complex partial and generalized tonic-clonic seizures have such negative effects on vocational, educational, social, cognitive, and psychological areas, and because these seizures can cause injury and even death, most epileptologists believe that AMTR should be offered to good surgical candidates sooner.
Uncertainty exists on how much time must elapse, or how many AEDs must be determined to be ineffective, before surgery is advised. As a result, the National Institutes of Health in the United States funded the Early Randomized Surgery for Epilepsy Trial, a huge prospective trial (ERSET). ERSET was created to compare AMTR versus two years of intensive AED treatment. The findings of ERSET should aid in addressing this issue.
Corpus callosotomy
The goal of this operation is to disrupt one or more key CNS pathways involved in seizure generalization, therefore lowering the frequency and severity of primary or secondary generalized seizures.
In general, corpus callosotomy appears to reduce the frequency of both primary and secondary generalized seizures (ie, tonic, clonic, tonic-clonic, and atonic seizures). Callosotomy improves atonic seizures greatly, although having atonic seizures does not indicate that a patient would benefit from surgery. Complex partial seizures can be substantially alleviated, but the consequences are significantly more erratic.
Some epileptologists argue that persons with mental disabilities who have epilepsy should not be considered for callosotomy since it seldom results in seizure freedom and these patients may benefit less than patients with normal intellect. Mental handicaps, whether present or absent, are not a reliable predictor of outcome. The authors have directly witnessed positive outcomes from callosotomy in individuals with mental disabilities.
Corpus callosotomy aims differ from those of resective surgery, when a seizure-free result is more likely and expectations are higher. Callosotomy is often used to minimize seizure frequency and related morbidity. Additional aims of social or occupational rehabilitation, which are appropriate to resective surgery, are frequently unrealistic following callosotomy.
Multiple subpial transection (MST)
The goal of this nonresective method is to eliminate epileptiform discharges and correlative seizures from the epileptogenic cortex by disturbing intracortical synchronization and so (theoretically) lowering or eliminating the seizure focus's epileptogenic potential.
The removal of the seizure-producing cortex from the brain has shown to be the most successful surgical therapy for partial (focal) seizures. This treatment, however, cannot be carried out if the seizure-producing cortex also provides an essential function, such as speaking. As a result, MST is the only surgically appropriate therapy for a focus within such cortex.
Functional hemispherectomy
The cortex is severed from all subcortical structures in this surgery, and the interhemispheric commissures are split, but the brain stays in situ.
In well-selected candidates with catastrophic epilepsy, functional hemispherectomy (commonly referred to as hemispherotomy in its present refined variants) is very successful for curing epilepsy. Candidates have damage and seizures that are restricted to one hemisphere of the brain. Their seizures are frequent enough to impair cognitive and reduce quality of life. The purpose of surgery is to separate the damaged hemisphere from the healthy hemisphere, allowing the latter to function normally without the weight of seizures or interictal discharges.
The majority of patients who have undergone hemispherectomy have been youngsters, while some past cases have included adults. Rasmussen encephalitis, other encephalitides, prenatal ischemia (often with porencephaly), Sturge-Weber syndrome, cortical dysplasia, hemiconvulsion-hemiplegia-epilepsy (HHE) syndrome, hemimegalencephaly, malignancy, and tuberous sclerosis are among the etiologies of catastrophic epilepsies leading to hemispherotomy
Pathology is preferentially restricted to a single hemisphere of the brain; recovery following surgical treatment is dependent on the remaining hemisphere's capacity to take up cognitive and linguistic skills that may have previously been within the domain of the afflicted hemisphere.
Delaying surgery can result in a decrease in cognitive function; growing research shows that seizures themselves might impede cognitive development. The timing of surgery is determined by the severity of the seizures, the natural history of the patient's sickness, and the patient's reaction to antiepileptic medication therapy.
When the condition appears early in childhood, many institutions advocate doing surgery as soon as possible to minimize cognitive impairment due to epileptic encephalopathy, which can impede learning and cognition. When it appears later in life, the scheduling of surgery might become more contentious. There is evidence, however, that individuals with late-onset disorders can react to surgery with improvements in neurologic function as well, suggesting that plasticity following hemispherectomy is not confined to children.
Postoperative complications that may occur include the following:
- AMTR – Hemiparesis, visual field deficit, infections, cranial nerve palsy, fever, verbal deficits and memory problems
- Corpus callosotomy – Hydrocephalus, aseptic meningitis, bleeding from the superior sagittal sinus, frontal lobe edema, venous infarction, and air embolism
- Functional hemispherectomy – Hemogenic meningitis, ventriculitis, cerebrospinal fluid leakage, and hydrocephalus; less commonly, stroke, infection, coma, and postoperative hemorrhage
Postoperative Care and outcome
A patient who has had anteromedial temporal resection (AMTR) is sent to the intensive care unit (ICU) for overnight observation, unless he or she can be returned to a seizure monitoring room on the epilepsy unit for attentive monitoring. On the night before operation, the patient sits by the bedside and conducts pulmonary toilet by deep breathing. If a fever develops, an incentive spirometer is utilized. The Foley catheter and arterial line are normally removed before the patient leaves the recovery room.
If a patient is maintained in the ICU overnight, he or she is transferred to a surgical floor the following morning. When the patient consumes oral fluids, the intravenous (IV) drip is switched to a saline lock. Ambulation, as well as sitting on a chair, is recommended. The patient is discharged on the third postoperative day, unless a complication emerges.
If the patient is taking numerous antiepileptic medicines (AEDs), an attempt is made to lower the dosages to nontoxic (but effective) levels, or to reduce the most poorly tolerated medication following surgery. If the patient remains seizure-free after around 2 years, the practitioner may address the benefits and drawbacks of quitting multiple AEDs with the patient. Patients are highly advised to maintain drugs for many years after surgery; there is a one-in-three probability of having a seizure in the five years following medication removal following epilepsy surgery.
A patient who has had a corpus callosotomy is monitored in the ICU throughout the first evening after surgery. During this period, neurologic markers may vary, making the disconnection syndrome more difficult. The patient may be unable to communicate or reply rapidly, and he or she may have inexplicable pupillary inequality. These results may necessitate computed tomography (CT) scanning to rule out a clot or tension pneumocephalus.
The patient's normal baseline neurologic state should begin to restore by the second postoperative day. The midsagittal plane of magnetic resonance imaging (MRI) is a good approach for determining the amount of sectioning.
Expected Outcomes
One randomized controlled study found that patients with medial temporal lobe epilepsy who have medication-resistant seizures (who have failed at least two AEDs approved for treatment of focal onset seizures at appropriate doses) benefit from antromedial temporal resection in terms of seizure outcome, even early in the course of their epilepsy. At the moment, patients must wait an average of more than 20 years before having AMTR.
What was not proved, due to the study's termination due to sluggish enrollment, was an improvement on quality of life. Other studies, however, have shown a considerable increase in quality of life in individuals who have been seizure-free thanks to surgery. One word of caution: a subset of patients who received dominant temporal lobectomy saw a statistically significant deterioration in verbal function on neuropsychological tests.
Several previous investigations clearly imply that the latter happens over time with chronic complexpartial seizures, either with or without development to tonic-clonic seizures. As a result, postponing surgery may not prevent language impairments and may expose the patient to all of the severe repercussions of ongoing seizures.
Conclusion
Seizures continue in around one-third of epileptic patients despite appropriate trials of various antiepileptic medications (AEDs). Despite this, many people with epilepsy never get seizure-free therapy. Epilepsy surgery is underused in industrialized, and especially in developing, nations, whether because to a lack of resources or because many clinicians are unaware of the existence of a curable disease.
In drug-resistant instances, epilepsy surgery should be explored before using a vagus nerve stimulator. Lesional epilepsy responds to drugs less well than cryptogenic/idiopathic epilepsy, although it has a greater likelihood of seizure independence following epilepsy surgery. A randomized controlled study proved the efficacy of temporal lobectomy for mesial temporal epilepsy.