Synovial Cyst
Overview
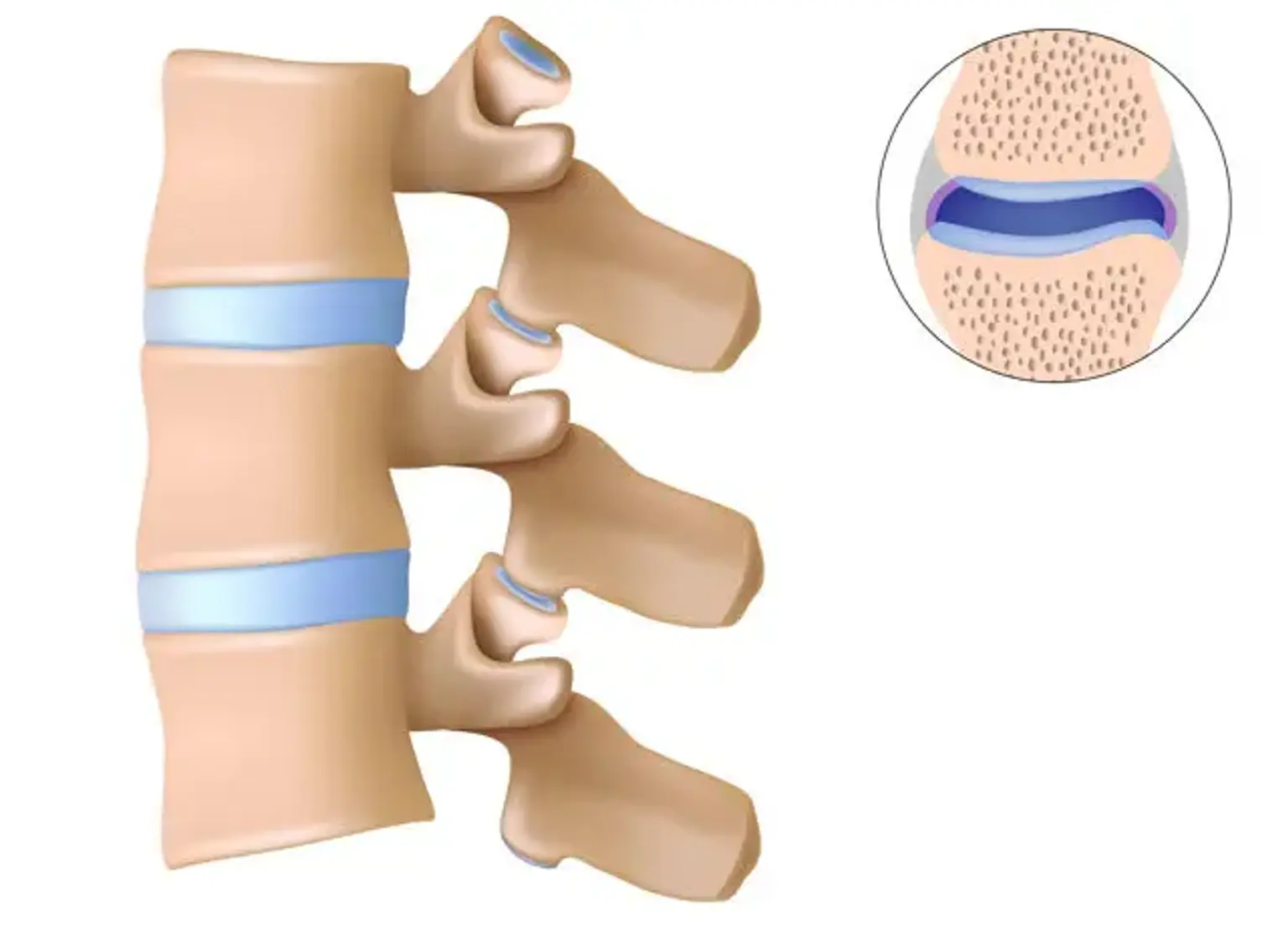
Synovial cysts are abnormal fluid-filled sacs that develop in the joints of the spine. These cysts are not malignant, as they are benign. Synovial cysts often arise as a result of aging-related degenerative changes. They can be found all the way up the spine, although they are most frequent in the lower back.