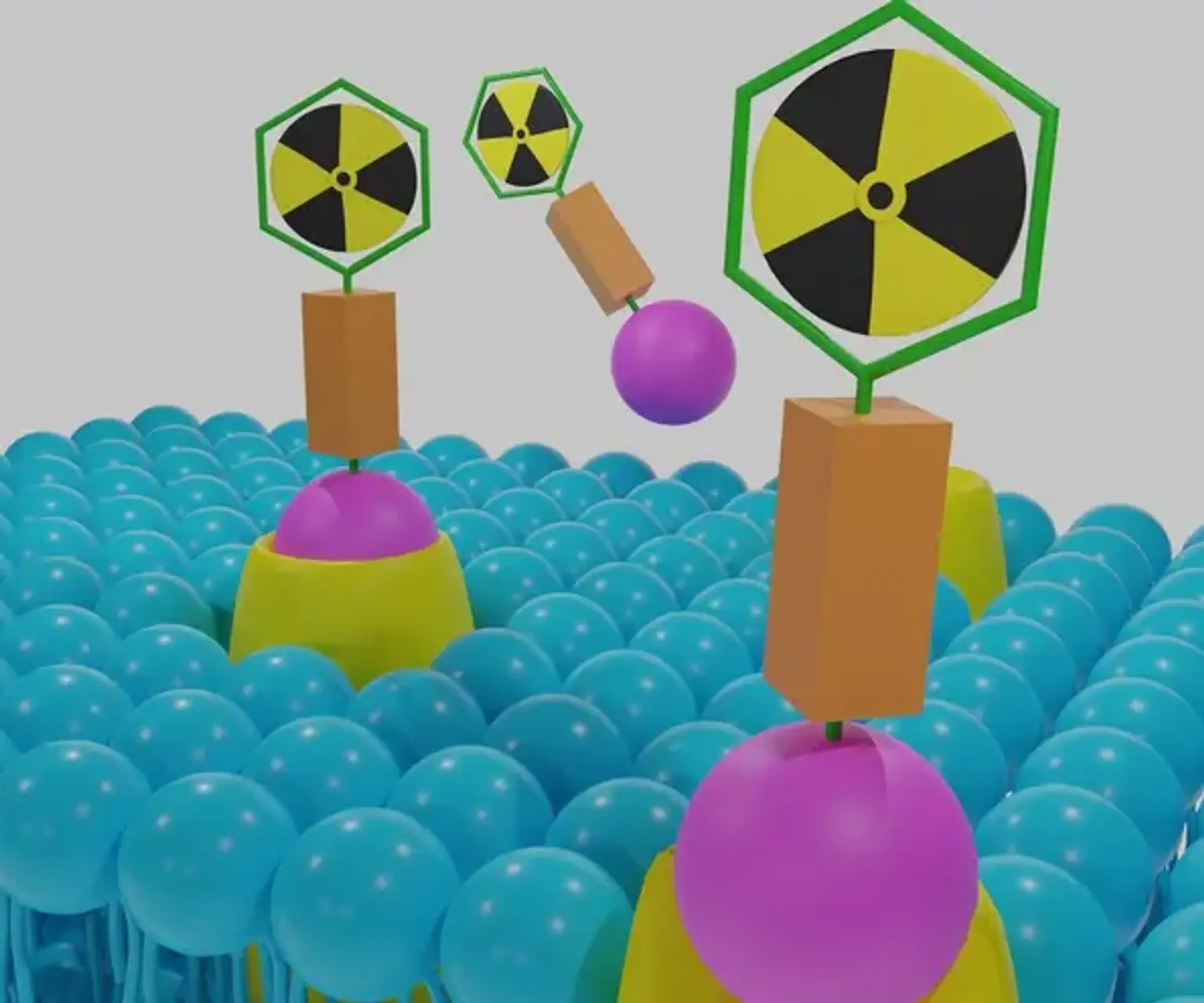
Targeted Radionuclide Therapies (Theranostics)
In nuclear medicine, stable and unstable isotopes, which do not undergo radioactive decay over time, are used for therapeutic purposes. In pharmacokinetic research, stable isotopes are mostly utilized as tracers to examine human metabolic processes. Since the tailored synthesis of novel carbon-13, nitrogen-15, and oxygen-18 radiolabeled compounds as well as noble gas isotopes is actively expanding, stable isotopes currently play a significant role in current medical research and have considerable potential for future research applications. Unstable isotopes are characterized by an overabundance of neutrons that interact with the protons in their nucleus, explaining both their ability to release ionizing radiation and their decay, as indicated by their half-life. A and/or an electron or positron emission, along with energy emission manifested as gamma rays (electromagnetic radiation), are generally used to stabilize radioisotope nuclei.
The current study examines radionuclide therapy in oncology and identifies emerging trends. A nuclear reactor's neutron activation process can create 3,800 radiation-emitting isotopes, as can other nuclear reactions in a cyclotron or linear accelerator. Less than 50 radioisotopes are routinely utilized in clinical settings, and about 200 have been studied for possible medical uses. Over 10,000 hospitals worldwide regularly employ radioisotopes for diagnostic purposes, with a prevalence of about 90%. More specifically, diagnostic nuclear medicine procedures are employed with a frequency of 2% per year in 26% of the world's population, or the approximate population of developed countries, with radioisotope therapy accounting for roughly one-tenth of these procedures. In the US, more than 20 million nuclear medicine procedures are conducted annually on 311 million people, compared to around 10 million procedures on 500 million individuals in Europe.