Thawing of Embryos (Optional)
Overview
After an in vitro fertilization (IVF) procedure, many couples choose to cryopreserve their frozen embryos. Due to concerns about ovarian hyperstimulation syndrome or excessive progesterone, they could freeze the embryos immediately after treatment before moving through with a transfer. Others save their embryos for later use or in case their first round is unsuccessful. In either case, each frozen embryo must be thawed in the same way before being used in a FET cycle. Many questions regarding the thawing process accompany the worry and excitement.
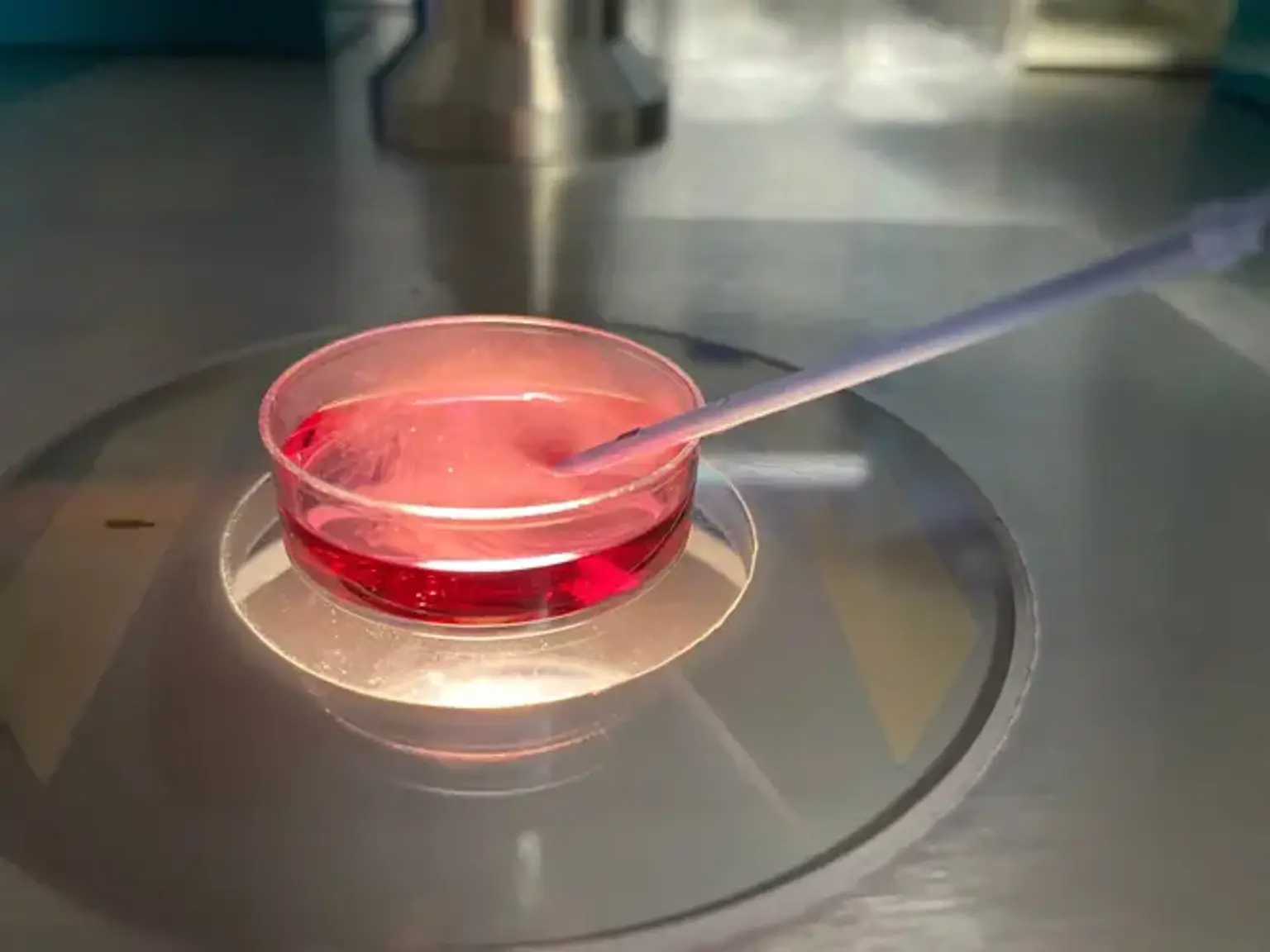
The opposite of freezing, embryo thawing entails bringing the embryos to ambient temperature before transferring them back into culture media at 37°C in a CO2 incubator. The embryos are then prepared for uterine implantation. On the day of the anticipated embryo transfer, the frozen embryos are reheated.