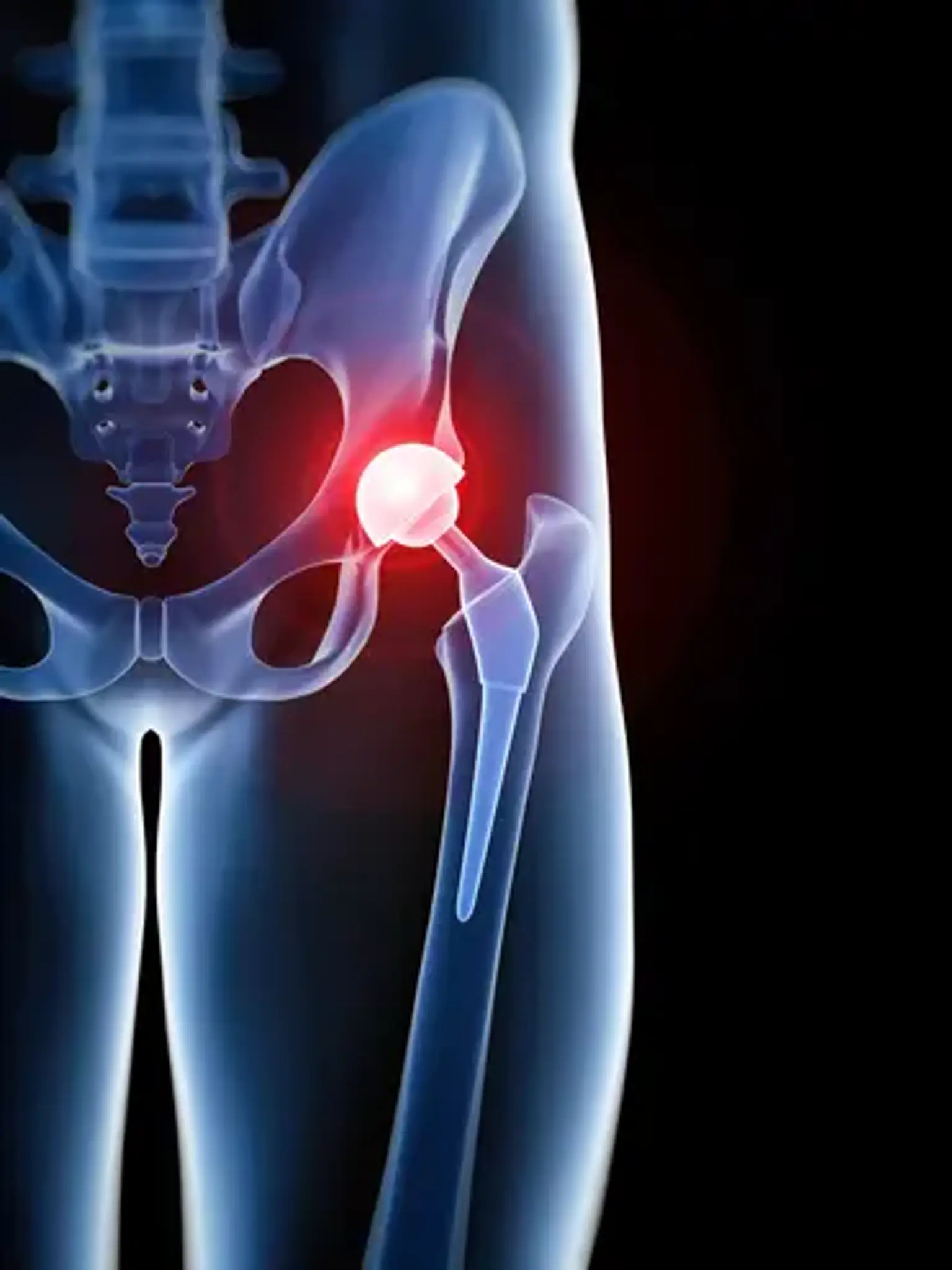
Total hip replacement
Overview
Walking or getting in and out of a chair may be uncomfortable and difficult if your hip has been injured by arthritis, a fracture, or other disorders. Your hip may feel stiff, making it difficult to put on shoes and socks. You could even feel uneasy while sleeping.
If drugs, changes in your daily activities, and the use of walking aids do not alleviate your symptoms, you may want to consider hip replacement surgery. Hip replacement surgery is a safe and successful operation that can reduce pain, enhance mobility, and help you go back to doing the things you like.