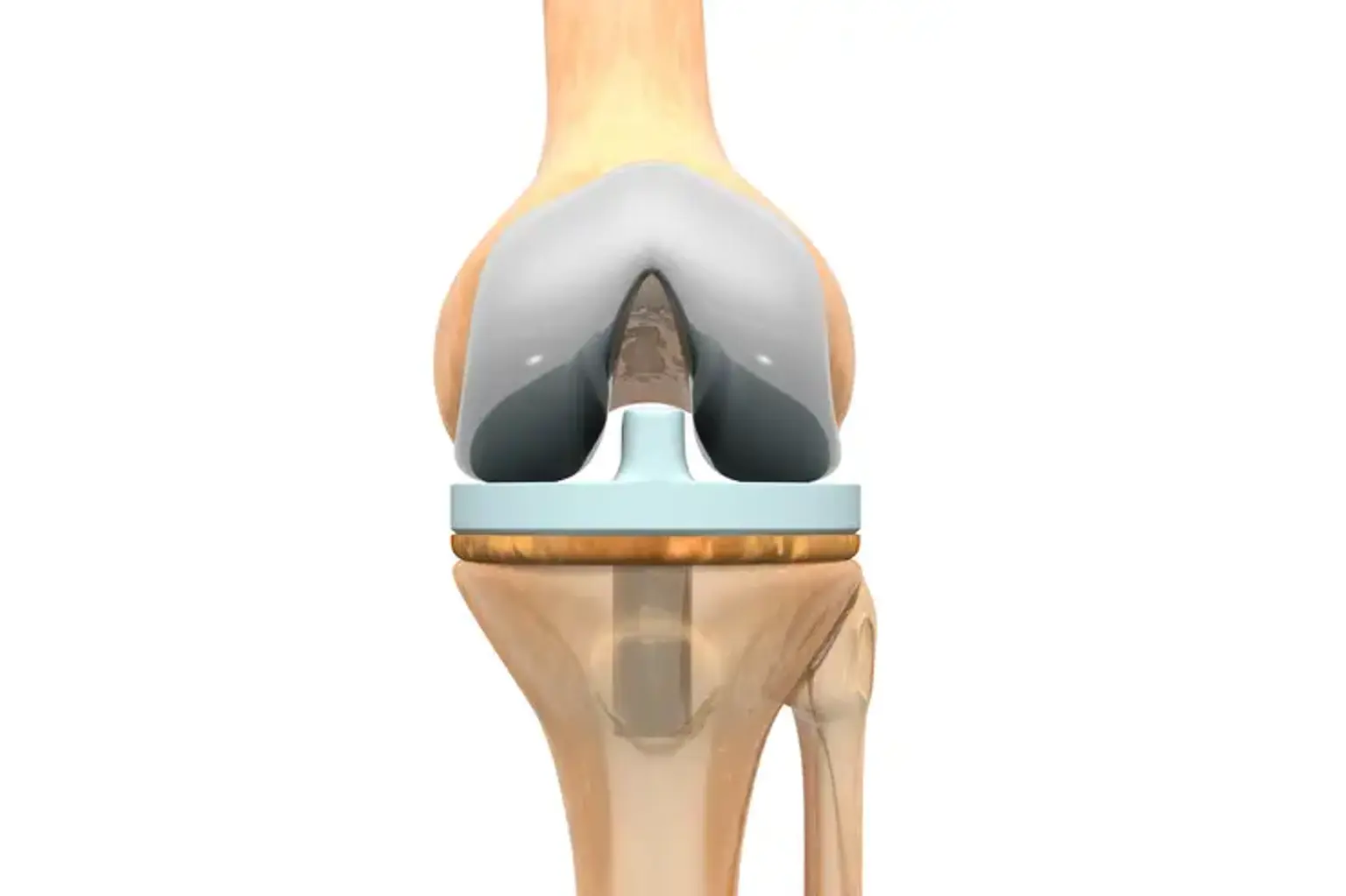
Total knee replacement
Overview
If your knee is significantly injured due to arthritis or injury, you may find it difficult to do simple activities like walking or climbing stairs. You may even have discomfort when sitting or lying down.
If nonsurgical therapies, such as drugs and walking aids, are no longer effective, you may wish to consider complete knee replacement surgery. Joint replacement surgery is a safe and successful technique for relieving pain, correcting leg deformity, and allowing you to return to regular activities.