Introduction
What is Laparoscopic Hysterectomy Surgery?
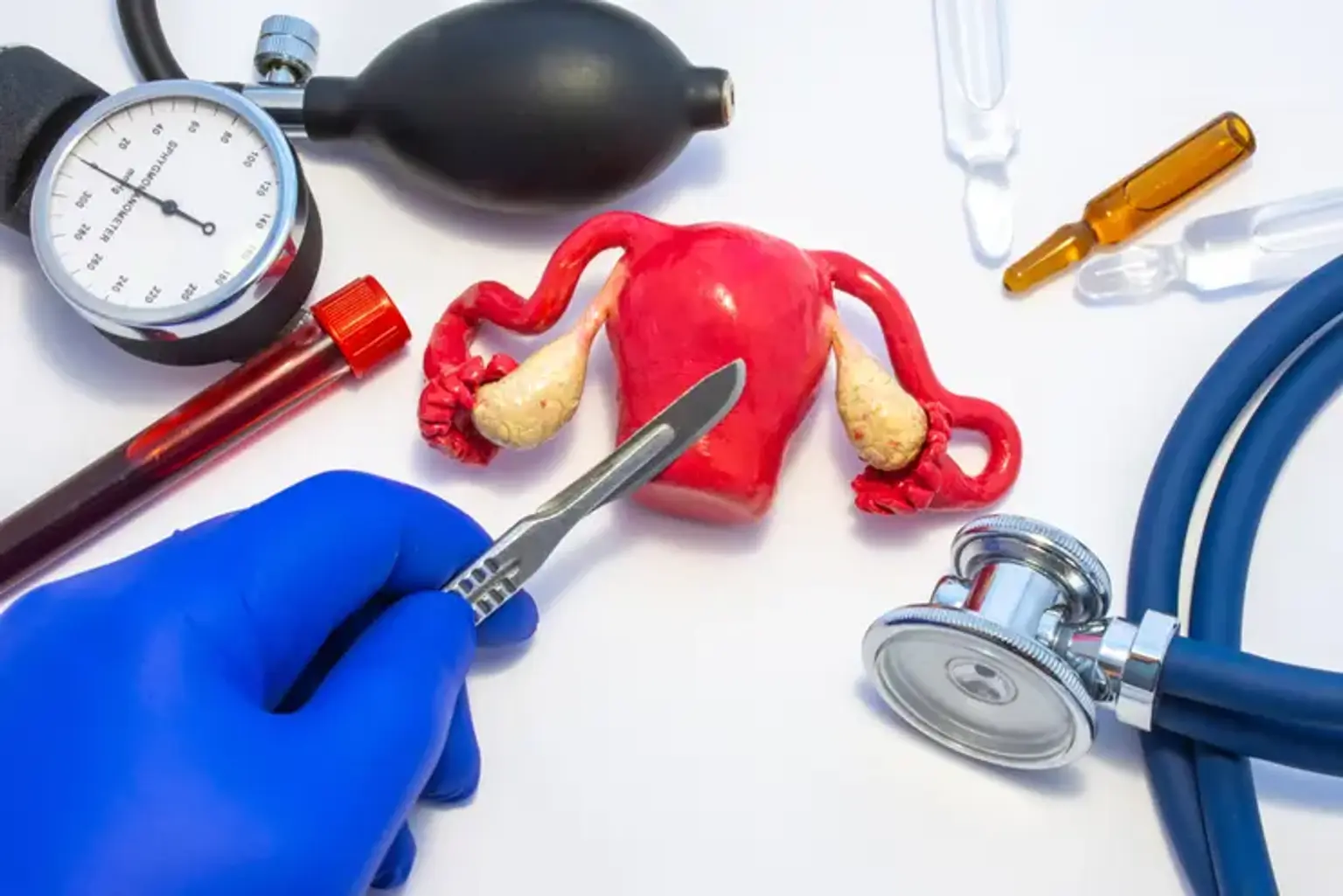
Laparoscopic hysterectomy is a minimally invasive surgical procedure used to remove the uterus. Unlike traditional open surgery, it involves making small incisions through which a camera and surgical instruments are inserted. This allows the surgeon to perform the operation with greater precision while minimizing trauma to the body.
Overview of Laparoscopic Surgery
Laparoscopic surgery, often referred to as "keyhole" surgery, uses small incisions, typically less than an inch long, to insert a camera and instruments. This technique has revolutionized many types of surgery, including gynecological procedures like the hysterectomy, offering patients faster recovery times and fewer complications.
Understanding Laparoscopic Hysterectomy
What is a Hysterectomy?
A hysterectomy is the surgical removal of the uterus. It is often recommended for conditions like uterine fibroids, endometriosis, chronic pelvic pain, or cancer. In some cases, the ovaries and fallopian tubes may also be removed, but this is not always necessary.