UL Inguinal Hernia (with Mesh)
Overview
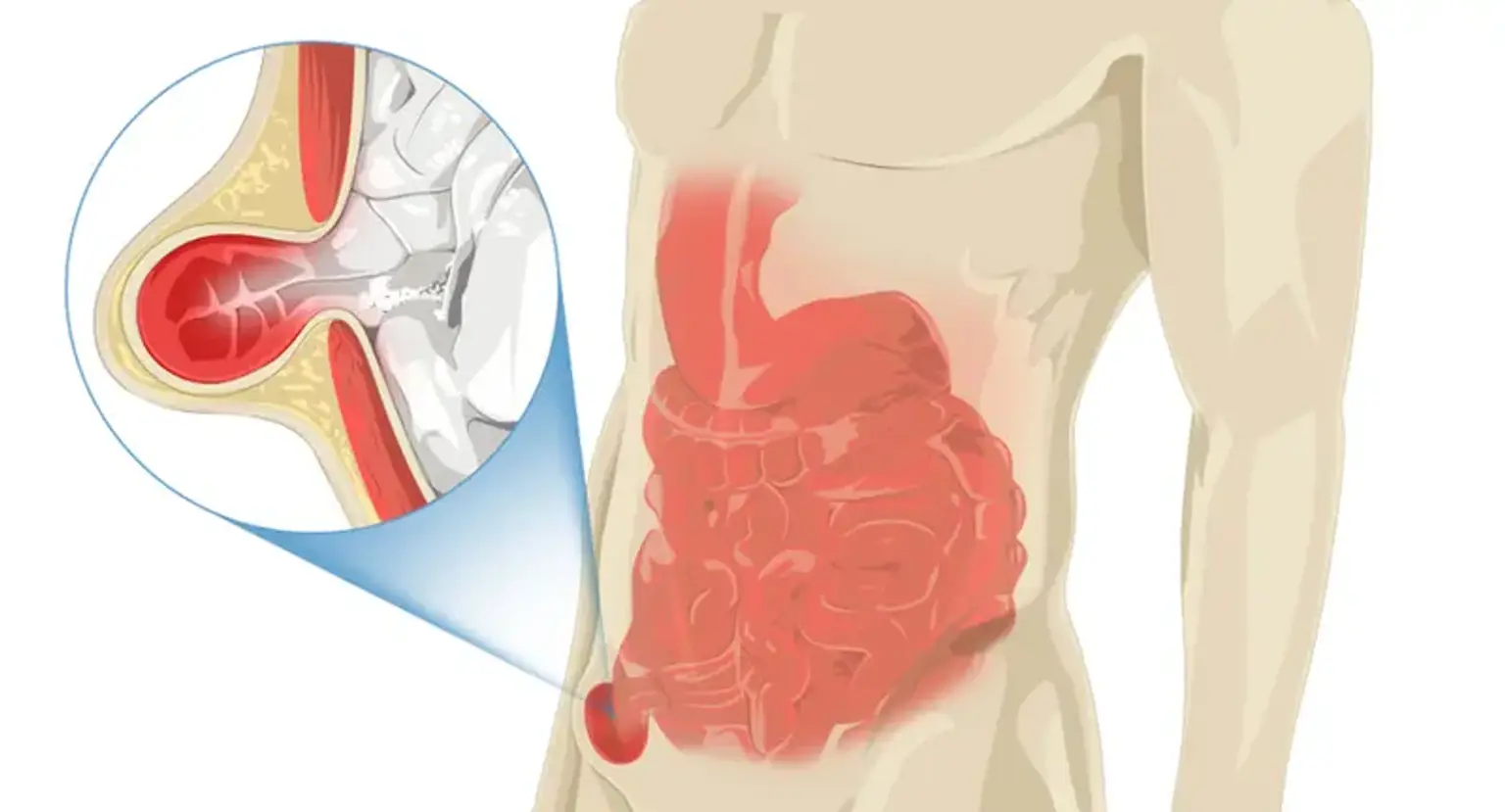
An inguinal hernia occurs in the groin, in a tube known as the inguinal canal. A protrusion on one side of your pelvic bone may be seen. Abdominal tissue pressing through a hole in your lower abdominal wall causes it. The gap might be congenital (existing at birth) or the result of typical, age-related muscle degeneration.
Inguinal hernias account for up to 75% of all hernias. Inguinal hernias affect around 25% of those assigned male at birth (AMAB), compared to 2% of those designated female at birth (AFAB). Middle-aged and older men are more likely to have direct (acquired) inguinal hernias. Indirect inguinal hernias afflict up to 4% of children, including 2% of AMAB newborns and 1% of AFAB babies.
Male groin hernias that do not produce symptoms do not require repair. Repair is often suggested in females because to the higher incidence of femoral hernias, which have more problems. Strangulation necessitates emergency surgery. Open surgery or laparoscopic surgery can be used to repair the defect. Open surgery has the advantage of being able to be performed under local anesthetic rather than general anesthesia. Following laparoscopic surgery, patients often experience less discomfort.