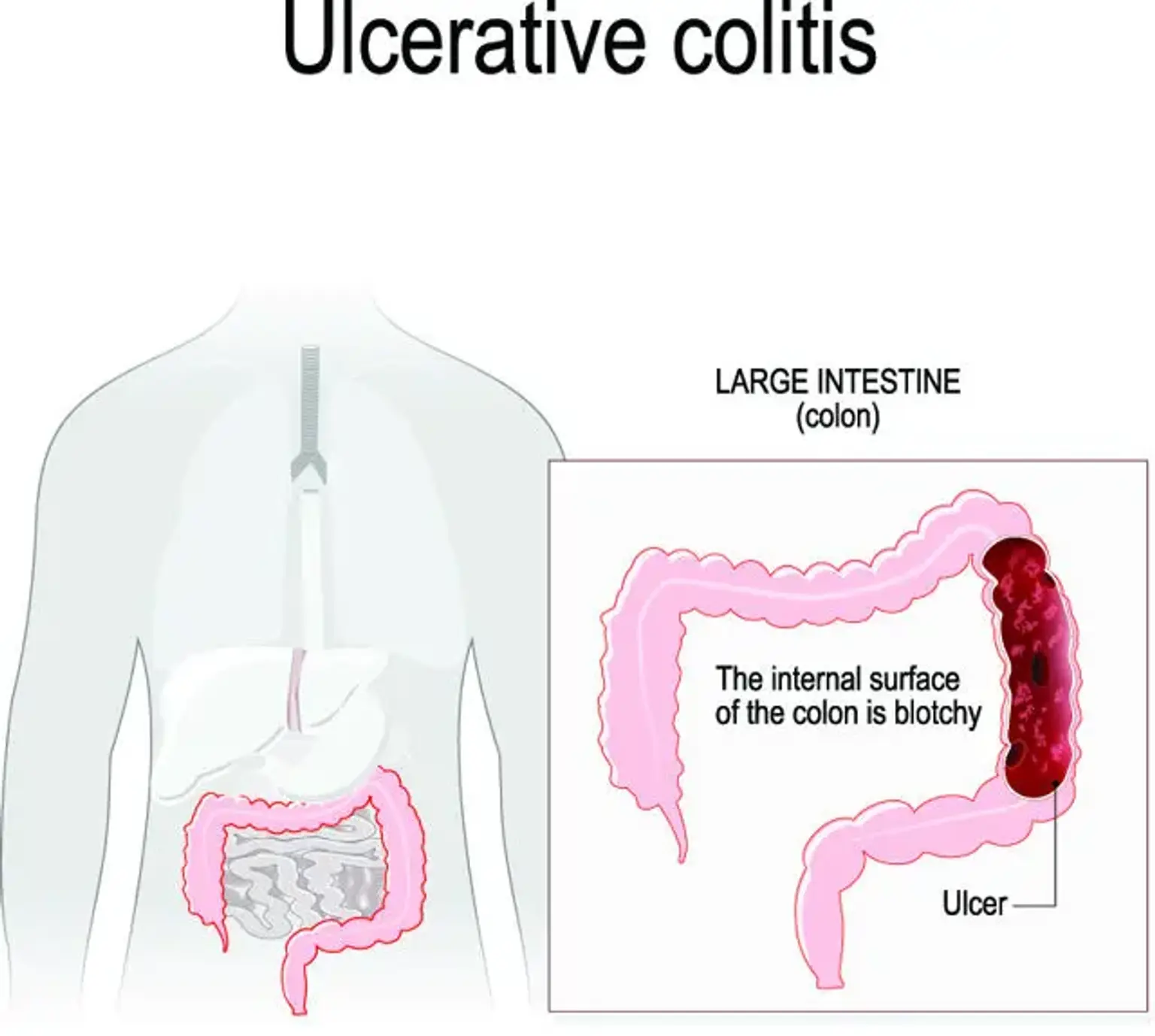
Ulcerative colitis
Ulcerative colitis (UC) is a medical condition that belongs to the inflammatory bowel disease (IBD) group. It is associated with inflammation, irritation, and ulcers or open sores that develop in the large intestines or colon. UC also results in bloody diarrhea, cramping, and a sense of urgency. These symptoms may sometimes wake a person up in the middle of the night to go to the bathroom.
With ulcerative colitis, the inflammation normally begins in the rectum, near the anus. This is where fecal matter exits the body. The inflammation may spread across the colon, affecting a section or the whole colon. The condition in which the rectum and lower section of the colon become inflamed is known as ulcerative proctitis.