Introduction
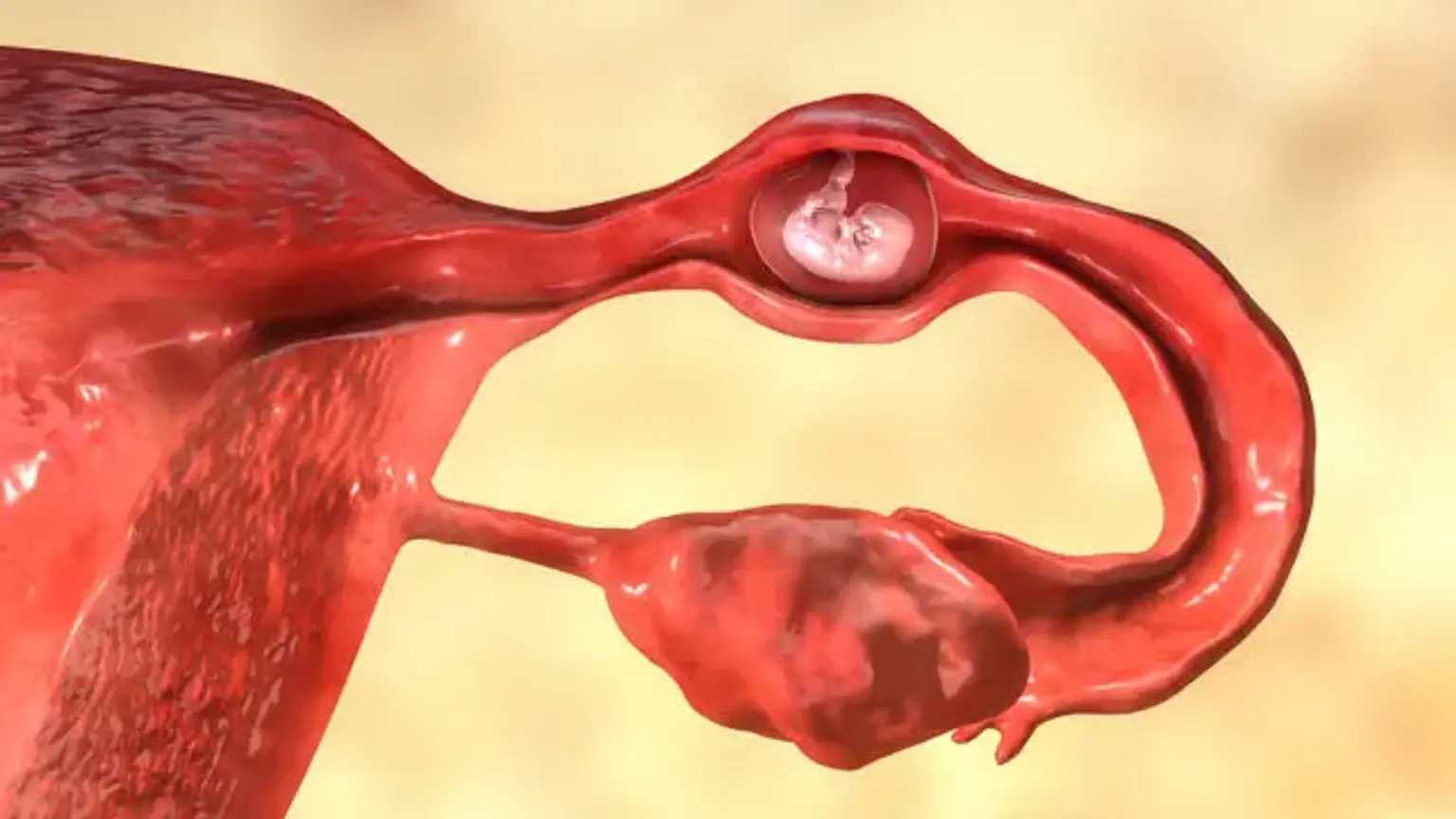
Unilateral fallopian tube removal, or salpingectomy, is a surgical procedure where one of the fallopian tubes is removed. This procedure is typically performed to treat specific health conditions, such as ectopic pregnancies, severe infections, or cancer affecting the fallopian tube. While it may sound daunting, many women who undergo unilateral fallopian tube removal continue to have successful pregnancies, as the remaining fallopian tube can often compensate for the loss of the other.
In this article, we’ll explore why and how the procedure is performed, what patients can expect during and after surgery, and the potential effects on fertility.
Indications for Unilateral Fallopian Tube Removal
Several medical conditions may necessitate the removal of one fallopian tube. These include:
Ectopic pregnancy: If a pregnancy implants in a fallopian tube, it can cause life-threatening complications. In such cases, removing the affected tube may be necessary to protect the woman’s health.
Severe infections: Chronic infections like pelvic inflammatory disease (PID) can damage the fallopian tubes, leading to scarring and blockage. If conservative treatments fail, a tube may need to be removed.
Tubal disease: Conditions like endometriosis can cause tubes to become blocked or damaged, impacting fertility.
Cancer: Cancerous growths in the fallopian tube, though rare, may require surgical removal to prevent the spread of the disease.
For women facing these conditions, unilateral fallopian tube removal can significantly improve their overall health and prevent further complications.