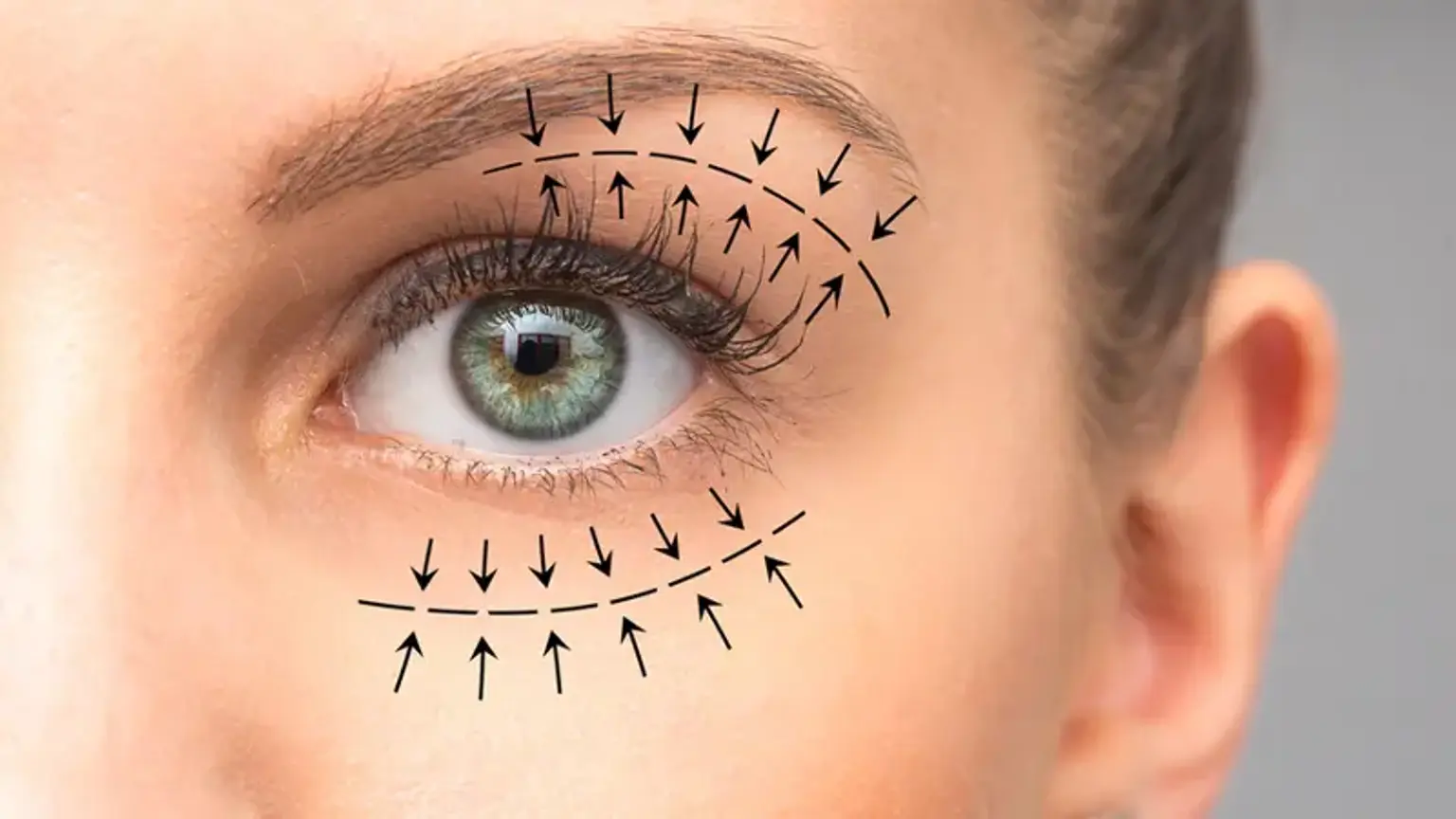
Upper Blepharoplasty
Due to the natural weakening of the skin, protruding fat pads, and sagging eyebrows, the upper and lower lids may change with age. Because the volume of the eyelids and the natural brow elevation varied from person to person, age-related eye changes can appear very differently. Some people's eyes become weary as they become older. The skin may drop over the natural crease of the eye, obliterating it. The skin may slide over the eyelashes and into the visual field in some situations. Blepharoplasty can treat the aesthetic and functional effects of loose eyelid skin.