Ureteral Reimplantation Surgery
Overview
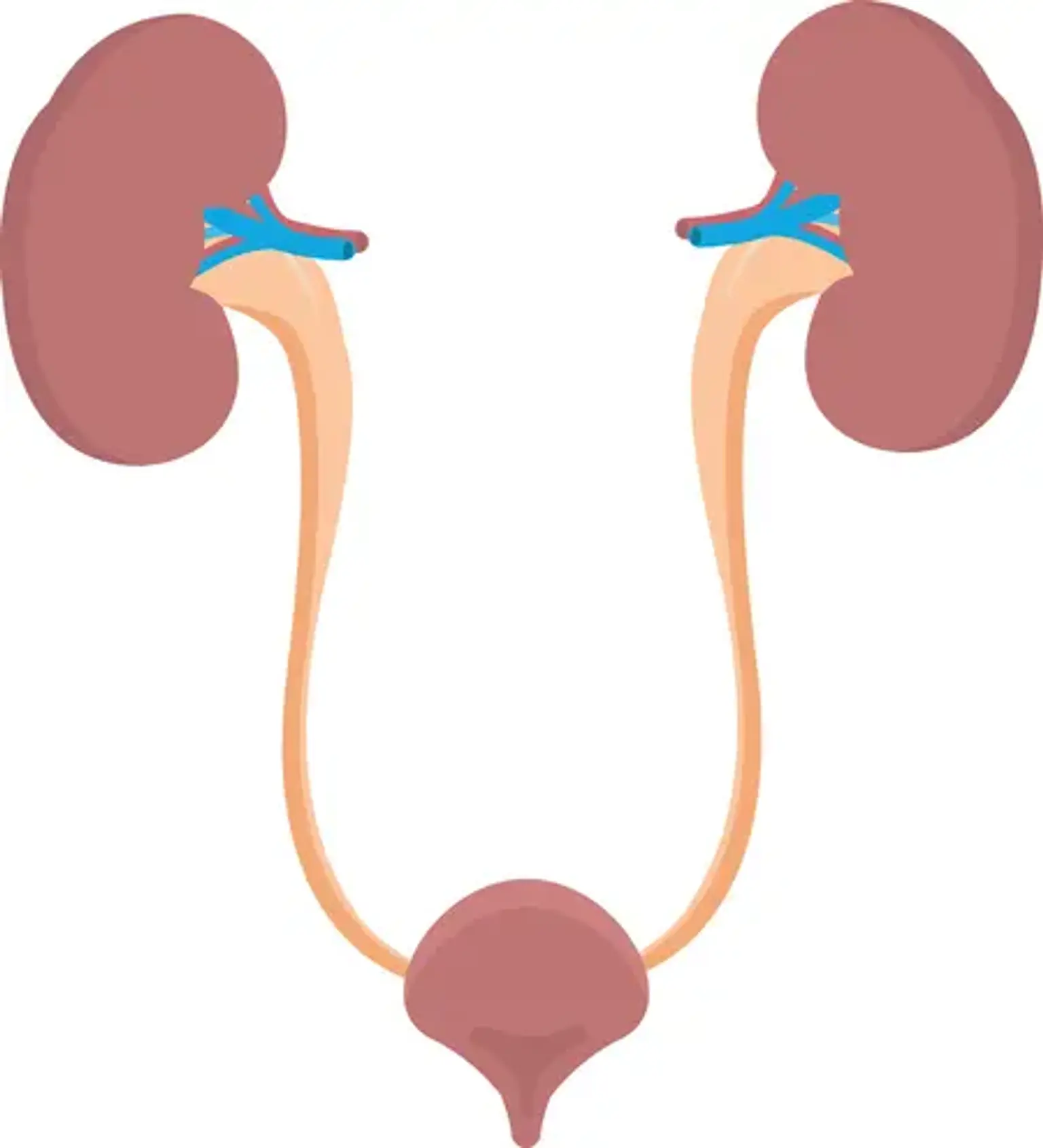
The ureter normally enters the bladder, which is formed of muscle, in such a way that urine may enter the bladder but not return up to the kidney. When the ureter enters the bladder improperly, the bladder's muscular backing does not completely cover the ureter, allowing urine to flow back toward the kidney. This is known as vesicoureteral reflux. Ureteral reimplantation is a surgical procedure that changes the location of these tubes where they enter the bladder wall, which aids in the treatment of reflexes. One (unilateral) or both (bilateral) ureters may require repair.