Vascular Malformations
Overview
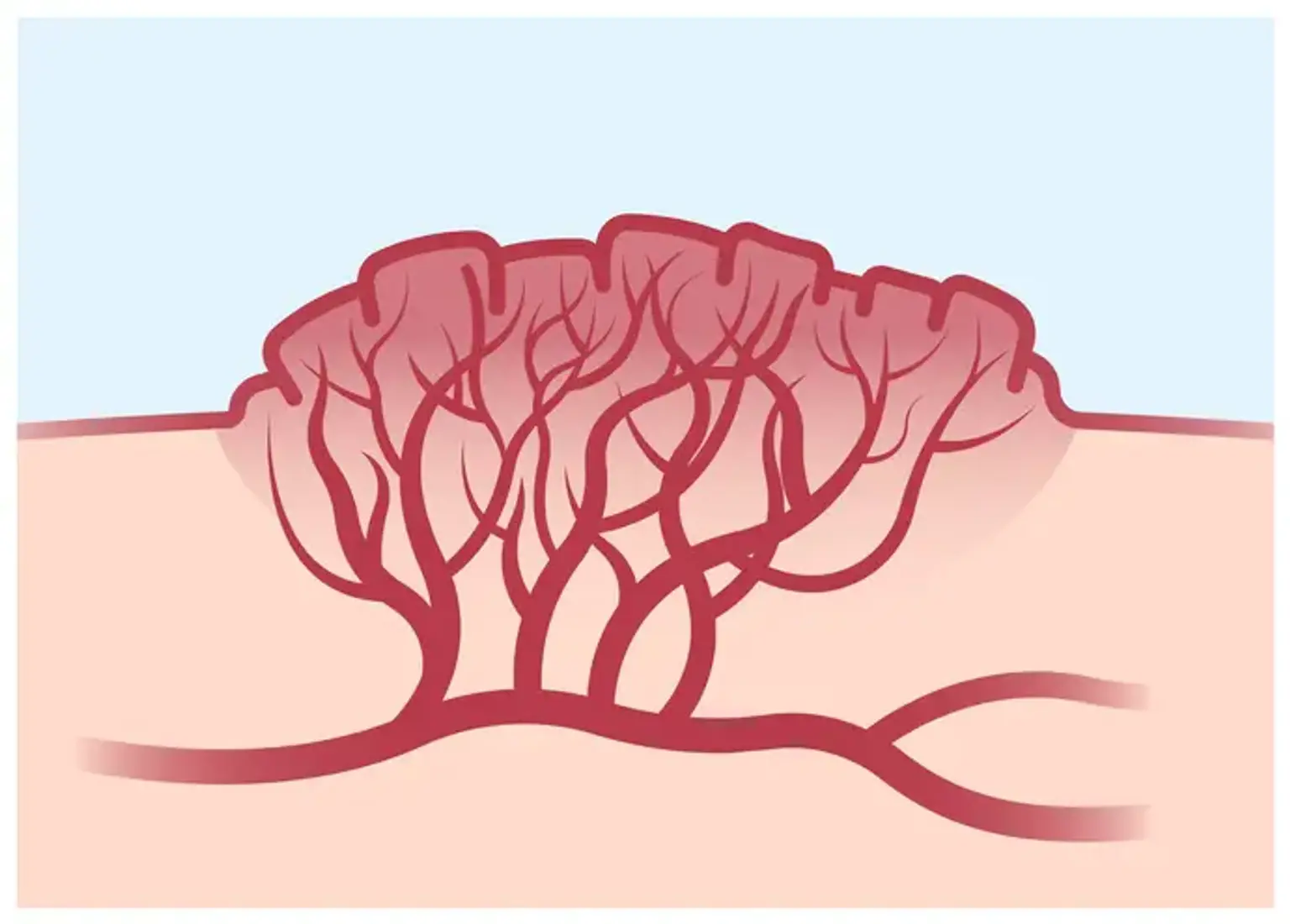
Blood vessel abnormalities, whether congenital or acquired, can affect arteries, veins, capillaries, lymphatics, and combinations of these blood vessels. Venous malformations and arteriovenous malformations are examples of vascular malformations, or arteriovenous malformations (AVMs).