Cerebrovascular Anastomosis
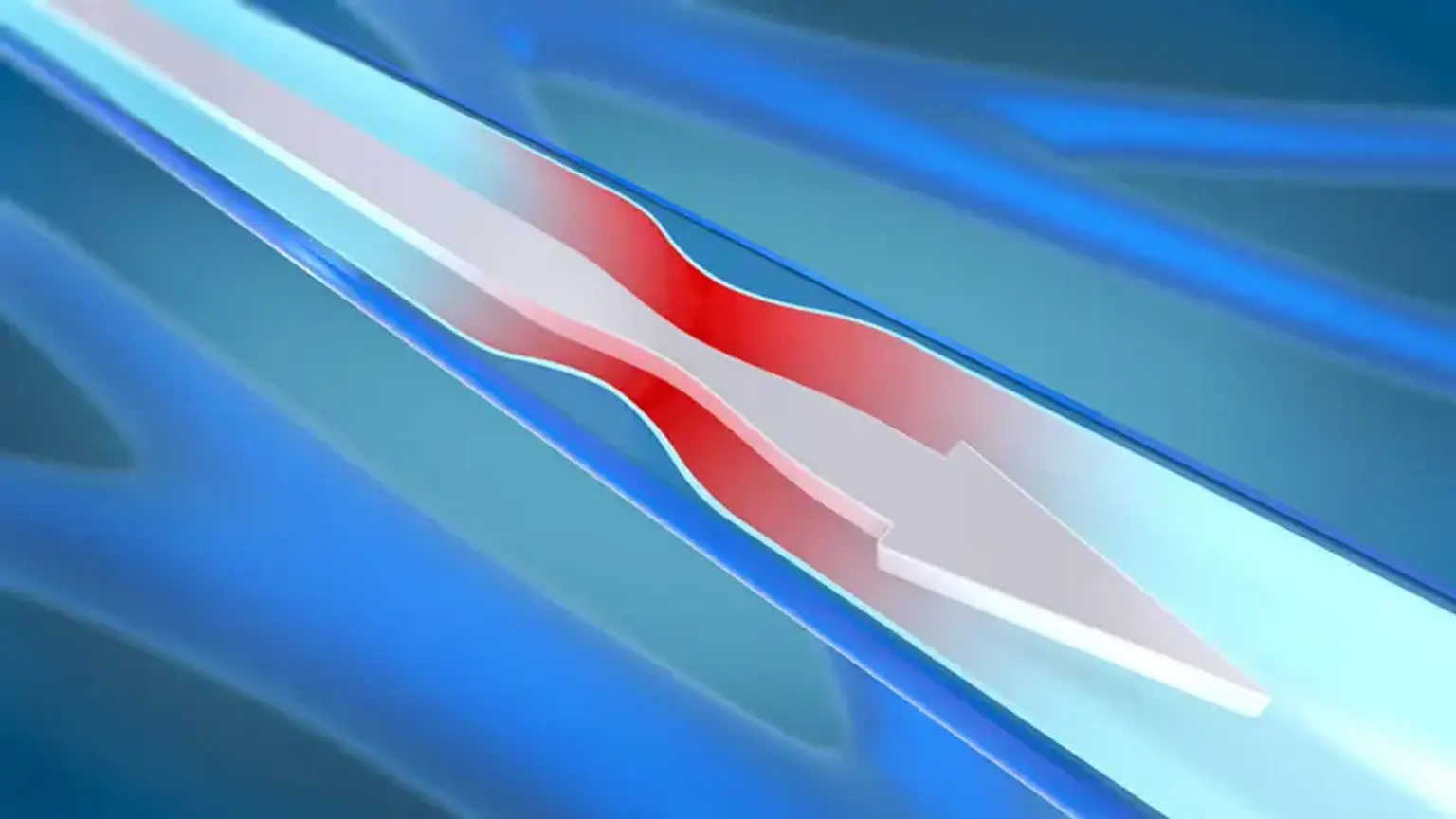
The goal of cerebrovascular anastomosis surgery is to revascularize or restore blood flow to the brain. The analog of a coronary bypass in the heart is a cerebral bypass in the brain. To reroute blood flow around a damaged or obstructed artery, surgery is performed to link a blood vessel from outside the brain to a vessel inside the brain. Bypass surgery aims to restore the brain's blood flow and fend against strokes.