Complex Coronary Interventions
Overview
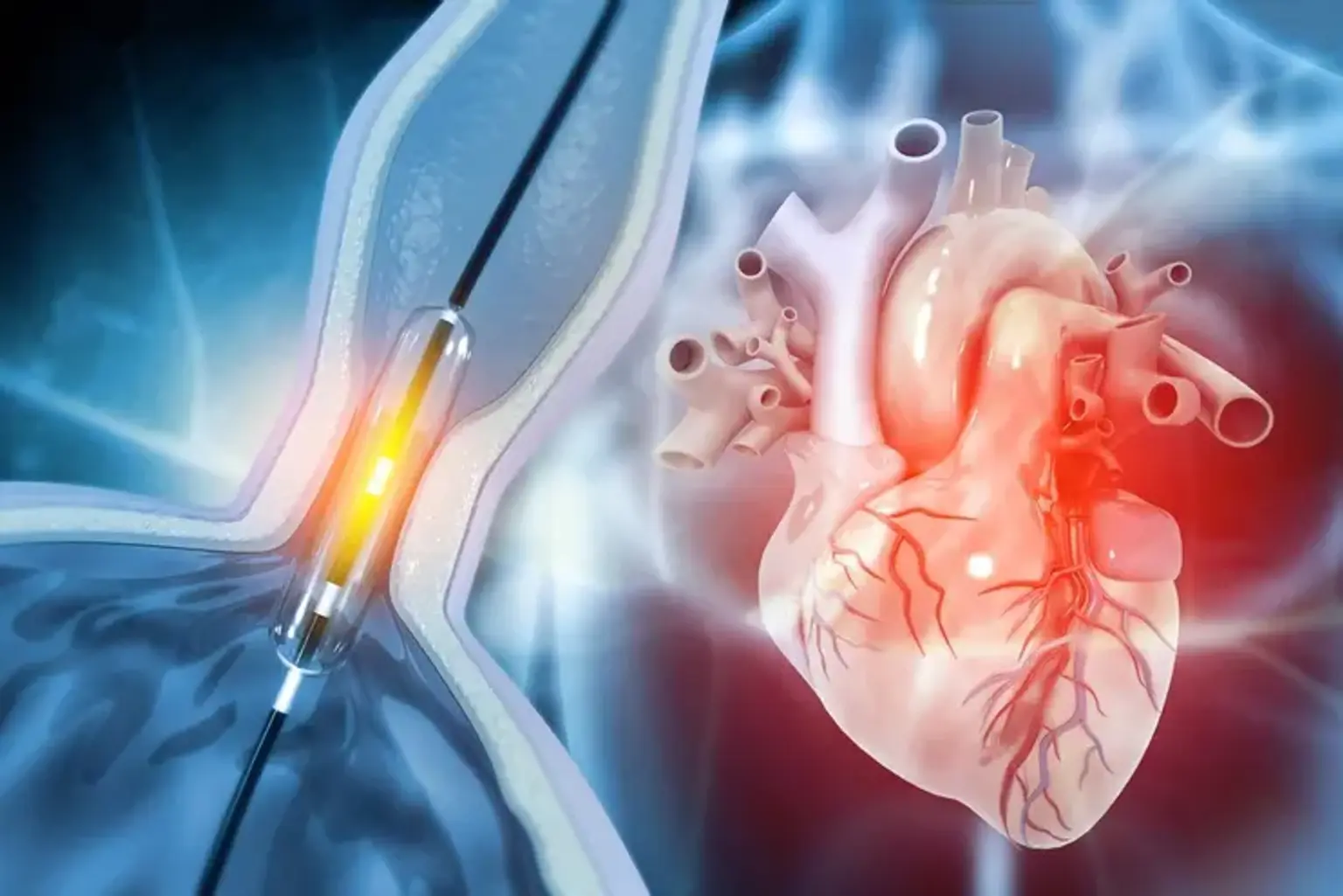
Chronic total occlusion (CTO) is a severe form of coronary artery disease in which the coronary arteries are completely (or nearly so) blocked by fatty deposits or plaque. Complex coronary interventions such as angioplasty and stenting can completely (or nearly completely) open clogged arteries.
In a complex coronary intervention, a fine angioplasty catheter is inserted into the affected coronary arteries. Using advanced imaging technology, one of our physicians will carefully guide the angioplasty catheter to the narrowest part of the coronary artery.
A wire with a ballooned tip will be inserted through the catheter, widening the narrowed artery and improving blood flow. The angioplasty balloon will then be removed, and a catheter with a closed stent will be inserted. He will then insert the stent into the artery, which will push against the artery's walls, acting as a support to keep it open. This procedure is minimally invasive and will not necessitate any large incisions.