CyberKnife Radiosurgery
Overview
Radio-neurosurgery reduces radiation exposure to healthy tissue surrounding the tumor. When compared to traditional radiosurgical procedures, the CyberKnife provides patients with various benefits, including immediate alleviation from pain and other problems.
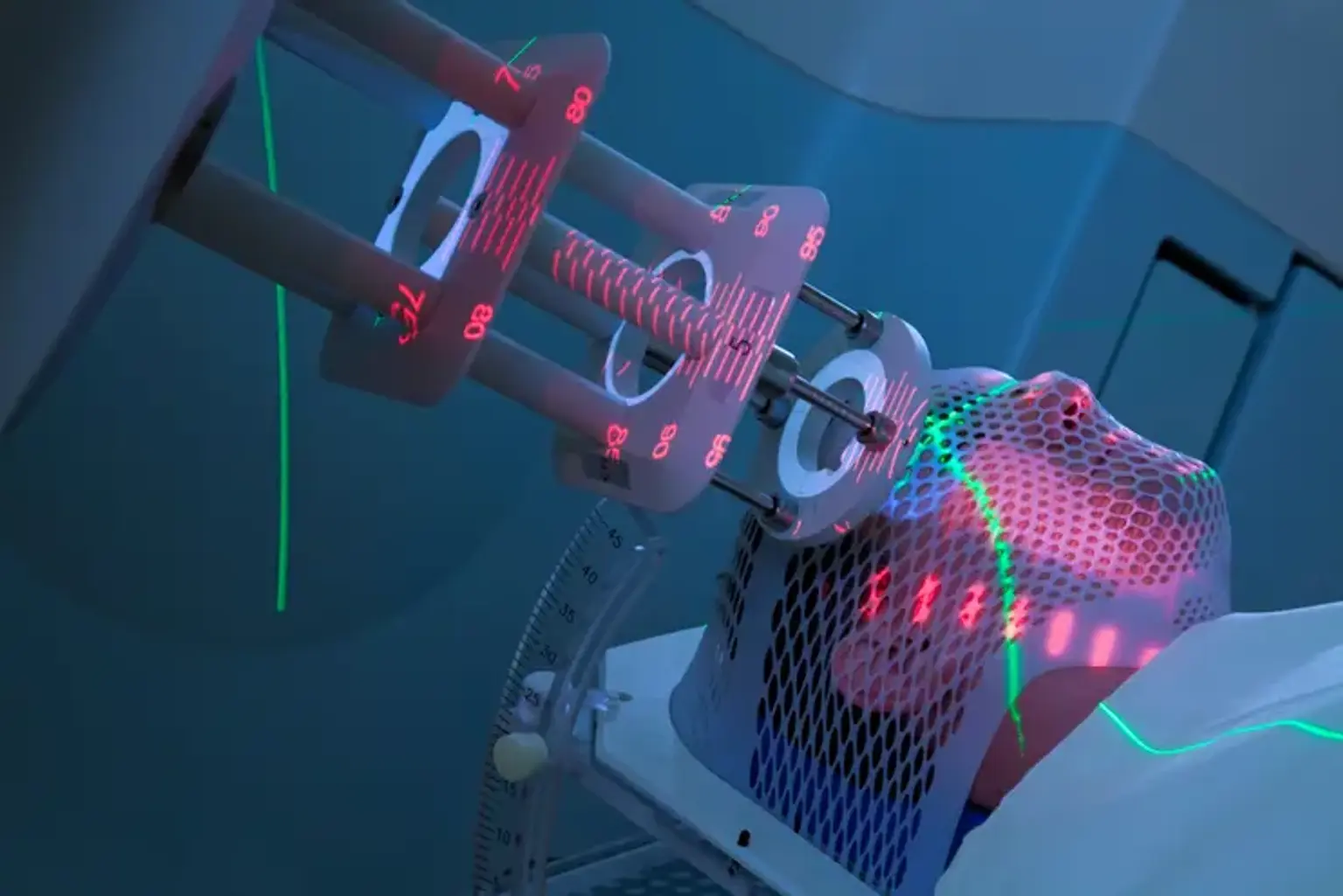
Treatments are given on an outpatient basis, with each session lasting 30 to 90 minutes. The number of treatments necessary varies based on the size, location, and form of the tumor, but normally just one to five daily sessions are required. The CyberKnife lets patients to lie comfortably on the operation table without anesthesia while the robotic arm glides to treat all parts of the tumor without touching them. Because of the low risk of complications and injury to good tissue, recovery is frequently quick.
Some disorders may be treated using the CyberKnife, a non-invasive radiotherapy device that similarly provides a single, carefully focused, high dosage of radiation. The CyberKnife is mostly used to treat minor benign or malignant brain tumors, epilepsy, trigeminal neuralgia, and aberrant blood vessel forms in the brain.