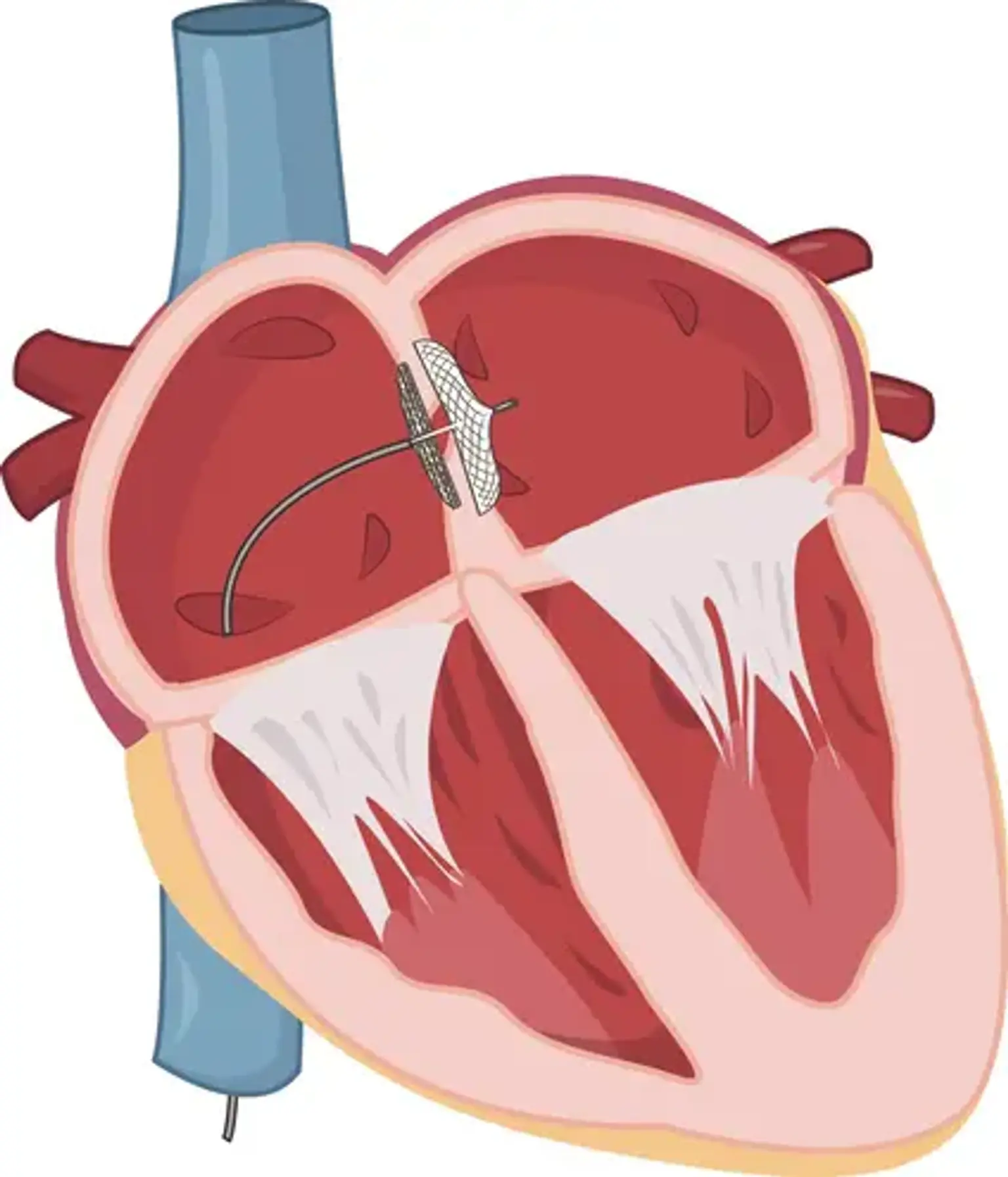
Device Closure of Atrial Septal Defect (ASD)
Overview
A common congenital cardiac problem, atrial septal defect (ASD), has a reported frequency of 1.0/1000 live births. Untreated ASD can lead to right ventricular overload and right heart failure, as well as atrial arrhythmias, systemic embolism, pulmonary hypertension, and mortality. Transcatheter closure of isolated secundum ASD has become the recommended therapeutic method in the majority of instances during the last 15 years. This technique has shown significant evidence of positive long-term effects at high-volume institutions.
ASD Secundum closure using transcatheter device is a mature technology that has been around for more than a decade. This therapy has become a widely acknowledged alternative to surgical therapy, and it is usually viewed as safe and successful.