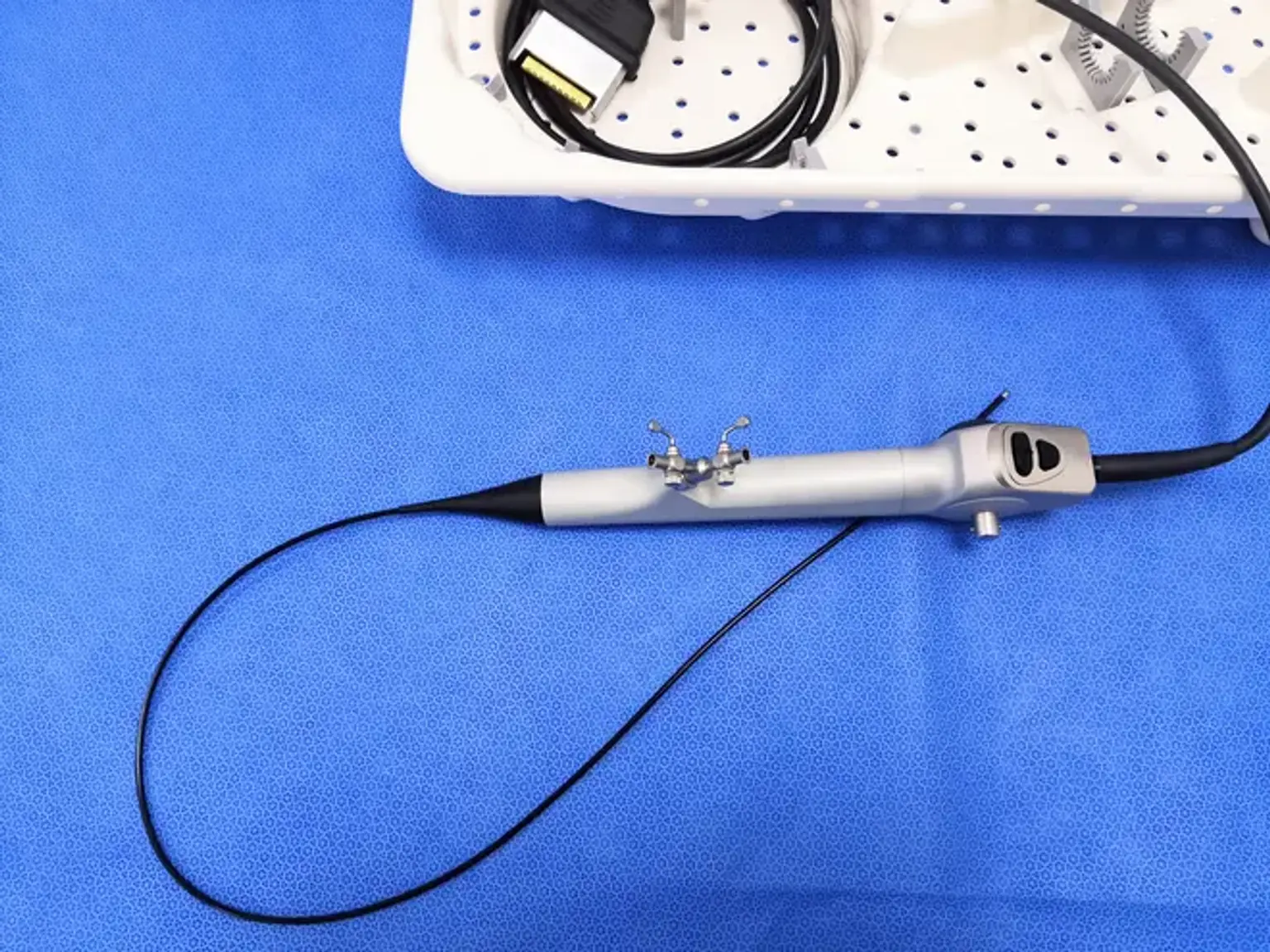
Direct Vision Internal Urethrotomy (DVIU)
Overview
A urethral stricture occurs when a scar caused by swelling, injury, or infection blocks or slows the flow of urine in this tube. A urethral stricture can cause pain in some people. The most common procedures for urethral stricture disease are direct visual internal urethrotomy (DVIU) and urethral dilatation.