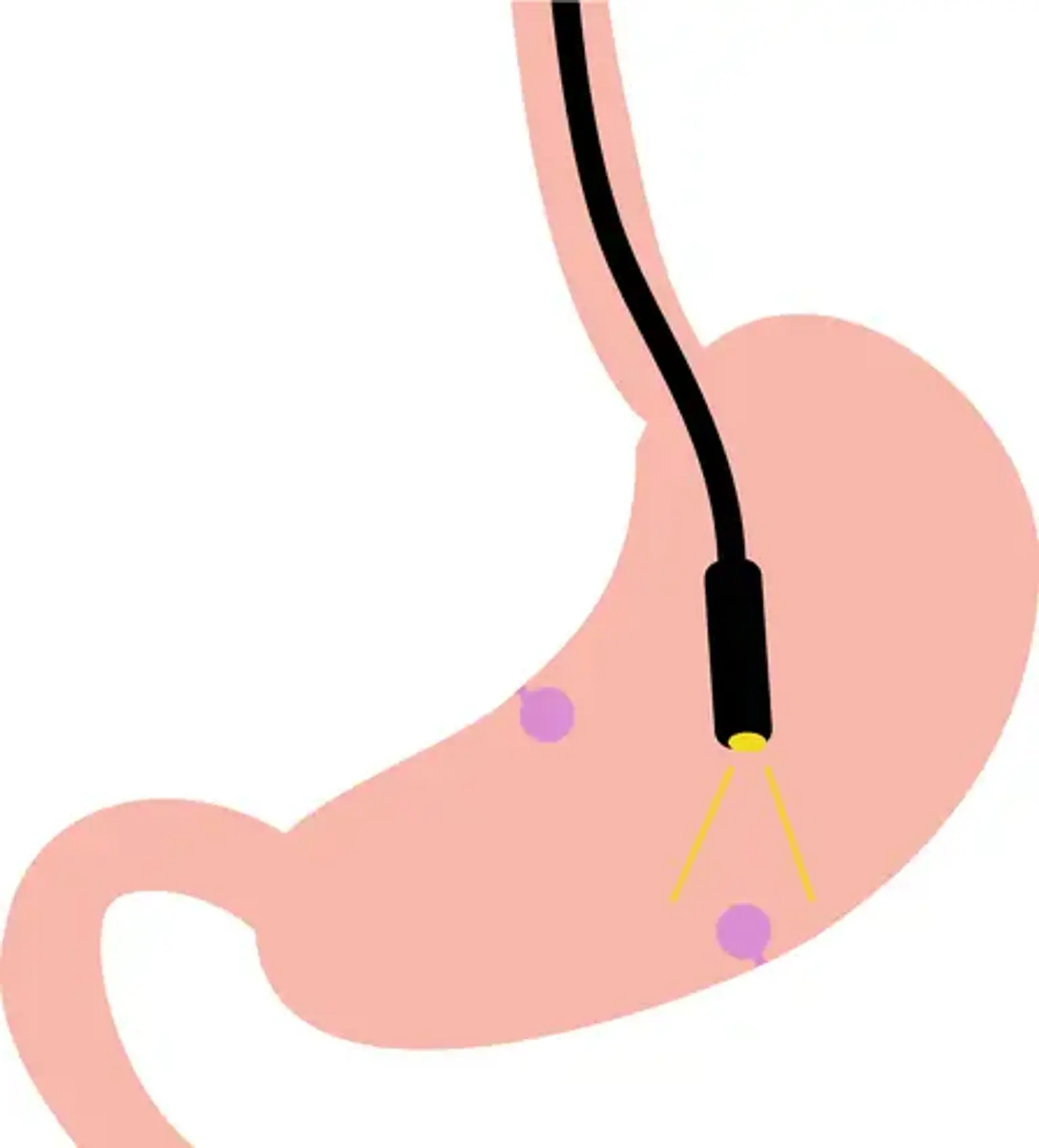
Endoscopic Submucosal Dissection (ESD)
Overview
Niwa and Tsuneoka et al. developed gastric polypectomy in the 1960s, and Wolff and Shinya described colon polypectomy for the first time in 1969. Endoscopic mucosal resection (EMR) was first used to treat early esophageal cancer in 1971 by Karita et al, Dyehle et al, and Inoue et al. Lesions under 2 cm in diameter can be removed in one piece during EMR; for lesions larger than 2 cm, only surgery or piecemeal resection were available. A minimally invasive and efficient method for en bloc resecting early-stage tumors or precancerous lesions in the gastrointestinal system that are larger than 2 cm is endoscopic submucosal dissection (ESD).
Endoscopic resection with a local injection of the hyperosmotic saline-epinephrine solution was a method created by Hirao et al in the 1980s. In this operation, the submucosa is dissected after a circumferential incision is created with a needle knife. Ono and colleagues at the National Cancer Center Hospital eventually formed an insulated tipped knife and began stomach ESD in the 1990s. Yahagi et al. employed the snare tip (later the flex knife and eventually the dual knife) for stomach ESD at the same time as Oyama began utilizing the prototype of the hook knife, which they made by bending a needle knife.
After more than 20 years, professionals can now safely conduct esophageal and colorectal ESD. However, without the proper indications, tools, and a well-thought-out plan, ESD cannot be carried out consistently and safely. Additionally, the initial step is to correctly locate and diagnose lesions that are amenable to ESD utilizing image-enhanced endoscopy. A minimal criterion is also to get sufficient histological specimens for thorough pathologic assessment with high-quality ESD.