Endovascular Coiling
Overview
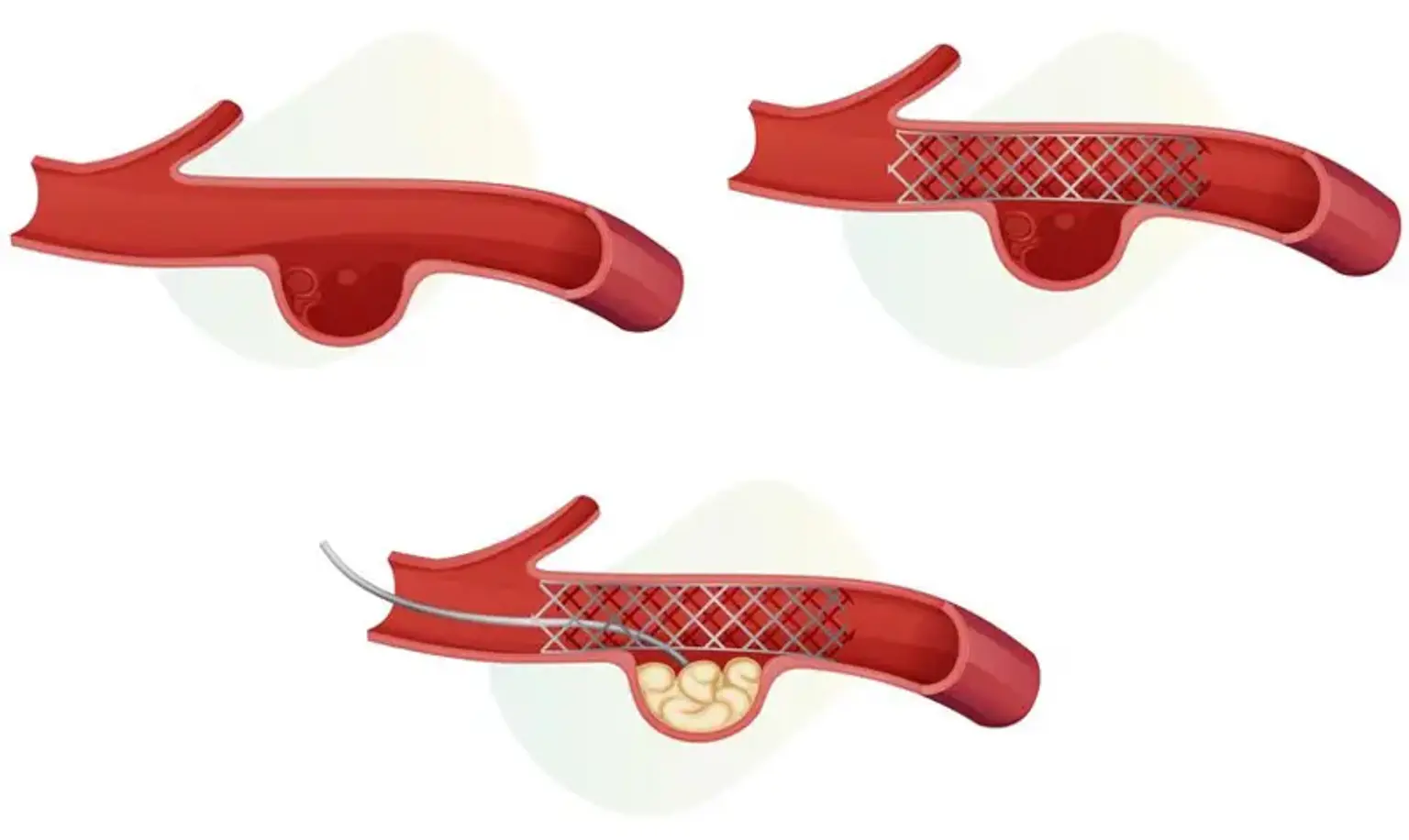
Endovascular coiling is a technique that is used to prevent blood flow into an aneurysm (a weakened area in the wall of an artery). Endovascular coiling is a relatively modern therapy for brain aneurysms, with patients having had it since 1991.
Endovascular coiling is a minimally invasive method that does not require a skull incision to cure a brain aneurysm. To access the aneurysm in the brain, a catheter is employed.
Endovascular coiling involves inserting a catheter via the groin into the artery containing the aneurysm. After that, platinum coils are released. The coils cause coagulation (embolization) of the aneurysm, preventing blood from entering it.