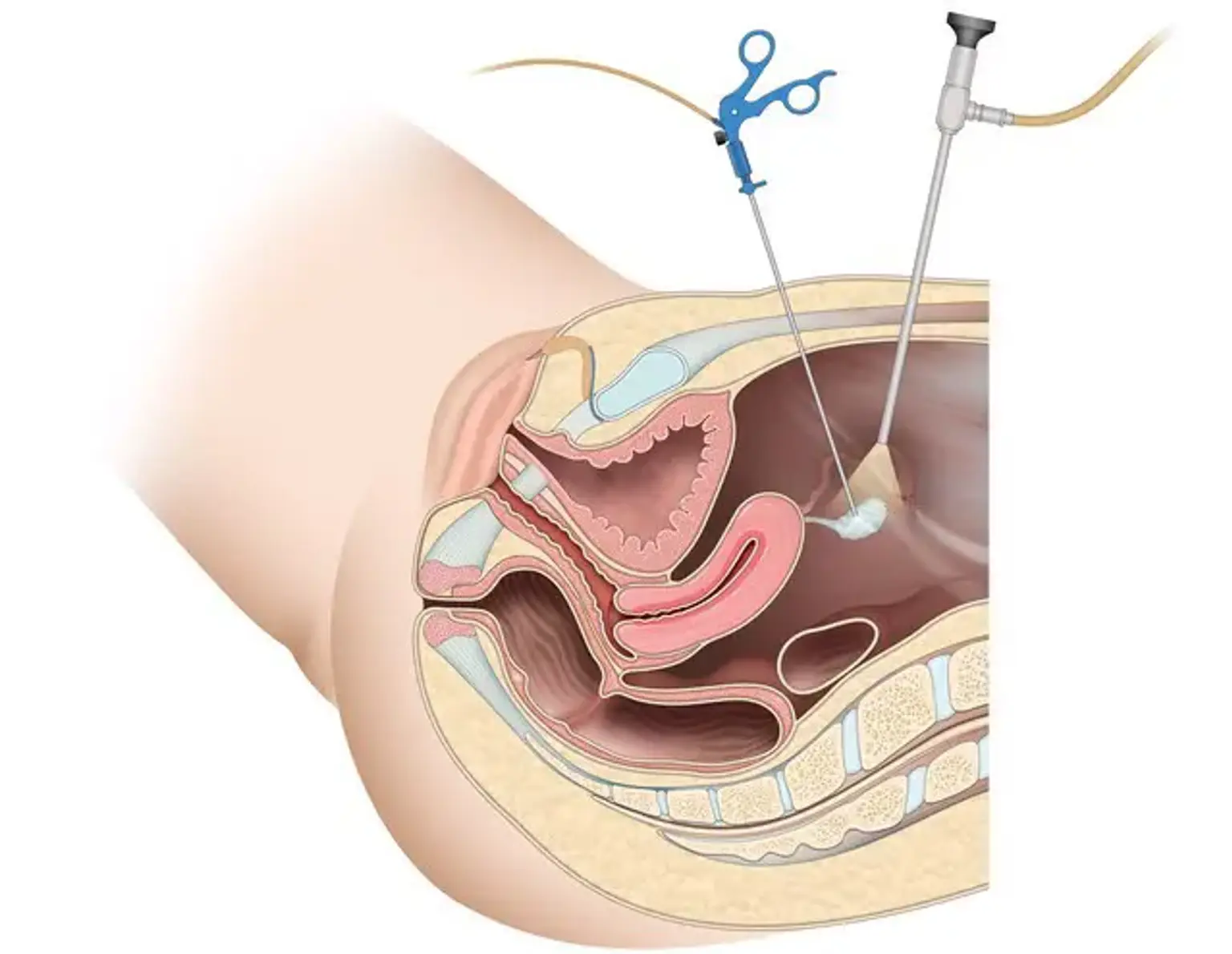
Gynecologic Laparoscopy
Overview
Laparoscopy has progressed from a restricted gynecologic surgical technique used only for diagnostic and tubal ligations to a significant surgical instrument utilized for a wide range of gynecologic and nongynecologic purposes during the last 50 years. Laparoscopy is becoming one of the most popular surgical procedures in many regions of the world.
Laparoscopy has become the treatment of choice for numerous gynecologic operations, including ectopic pregnancy removal, endometriosis therapy, ovarian cystectomy, and hysterectomy. Multiple studies have demonstrated that laparoscopy is safer, less costly, and has a quicker recovery period than laparotomy. Other treatments, such as myomectomy, sacral colpopexy, and the diagnosis and therapy of gynecologic malignancies, are benefiting from the laparoscopic technique.