Holmium Laser Enucleation of the Prostate (HoLEP)
Overview
What is benign prostatic hyperplasia (BPH)?
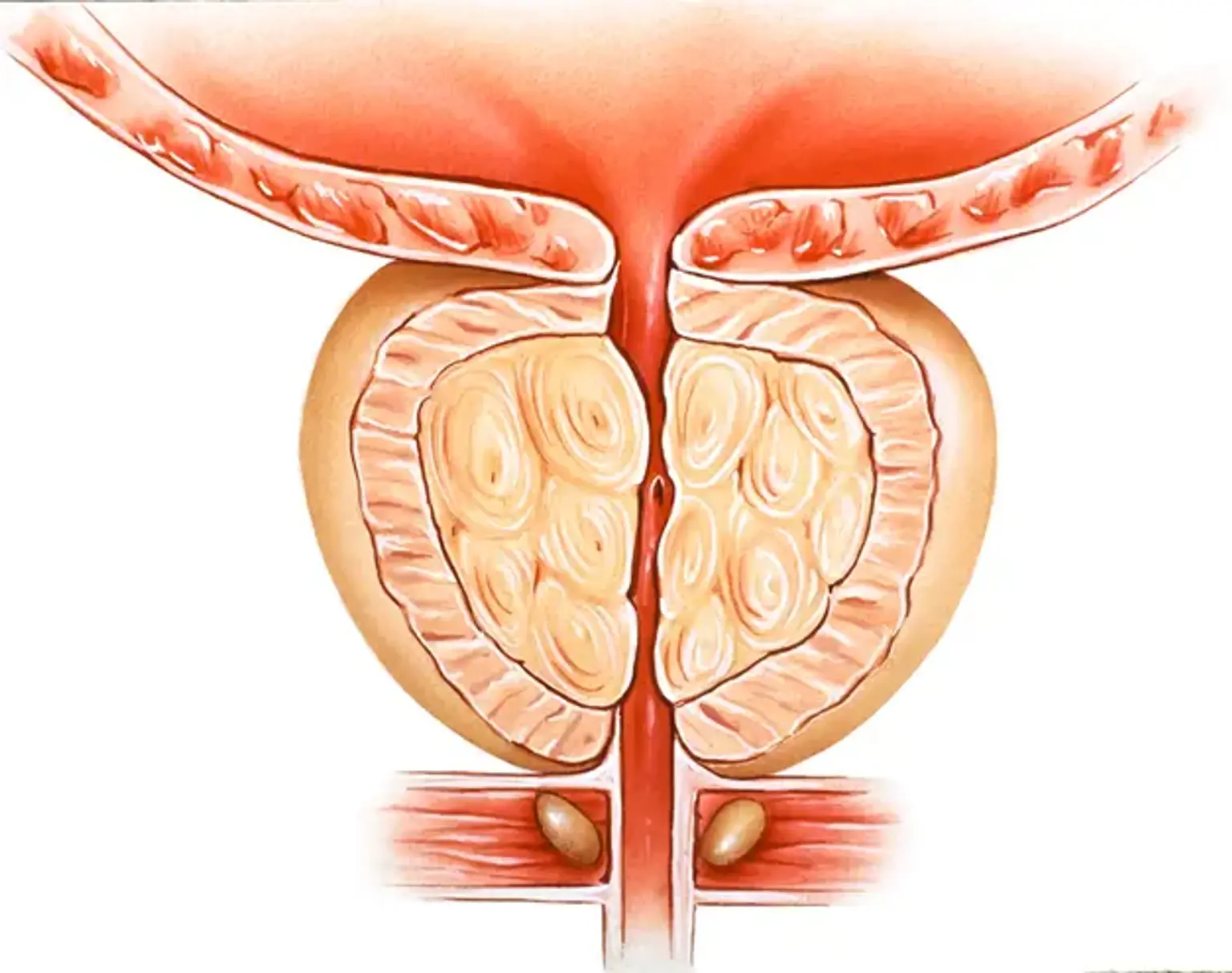
In males, the prostate gland is located just below the bladder and encircles the upper section of the urethra (a tube that drains urine from the bladder). The major function of the prostate is to release seminal fluid (the fluid that nourishes and transports sperm).
Benign Prostatic Hyperplasia (BPH) is a histopathological term for benign enlargement of the prostate gland caused by the growth of glandular epithelial tissue, smooth muscle, and connective tissue inside the gland.