Invasive Cardiology
Overview
Few things in life are as important as heart health when it comes to living a healthy lifestyle and having the best quality of life achievable. In addition to a healthy diet and regular exercise, visiting a cardiology clinic is essential.
However, genetics and family history are important predictors of whether or not you may develop heart disease. As a result, despite your best efforts, you may still have cardiac problems. It is critical to understand the differences between various forms of cardiac care.
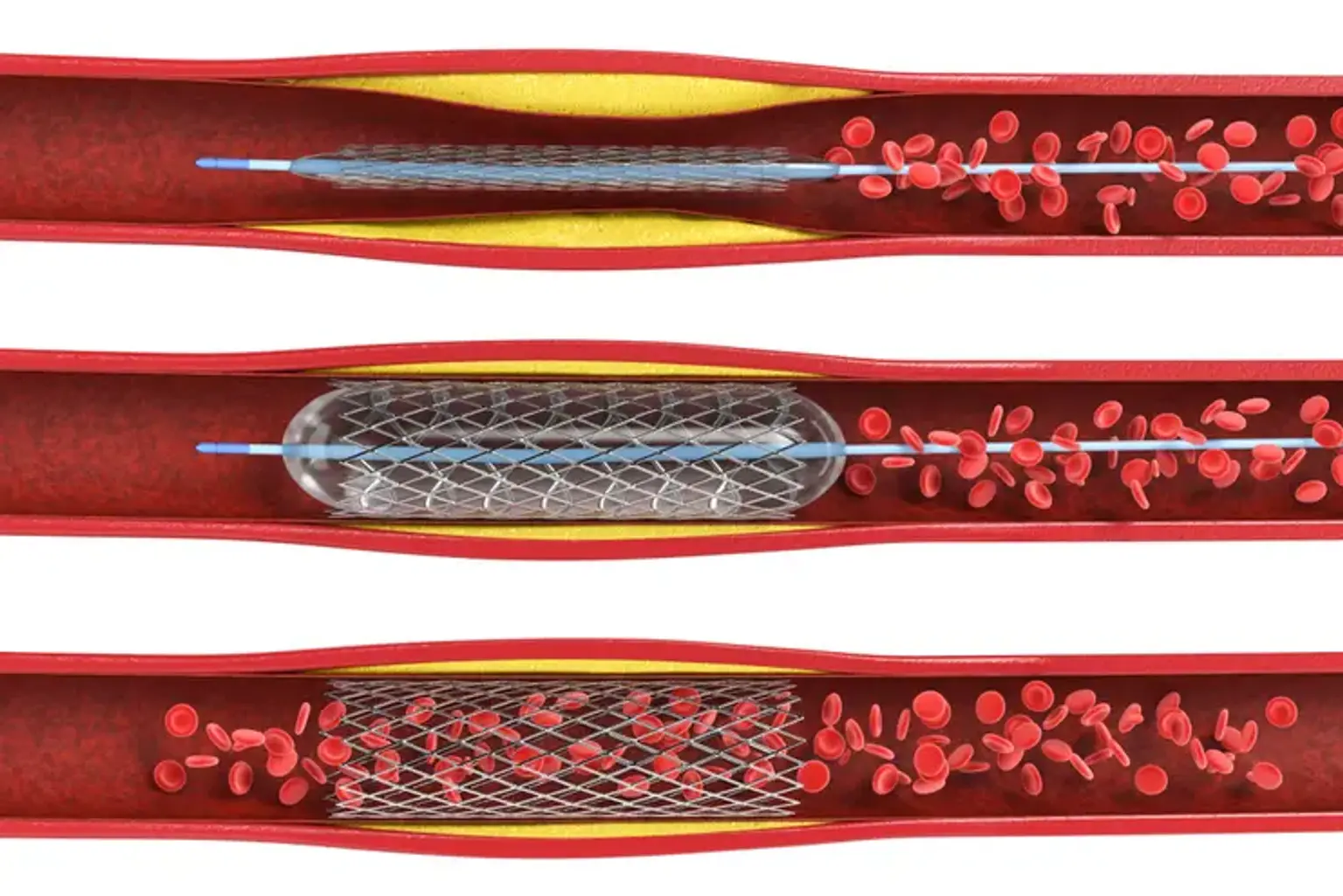
The phrase "invasive cardiology" refers to open heart or minimally invasive surgical techniques used to treat heart diseases and disorders. Angioplasty and coronary stenting are two examples of invasive cardiology techniques.