Intrauterine Insemination (IUI)
Overview
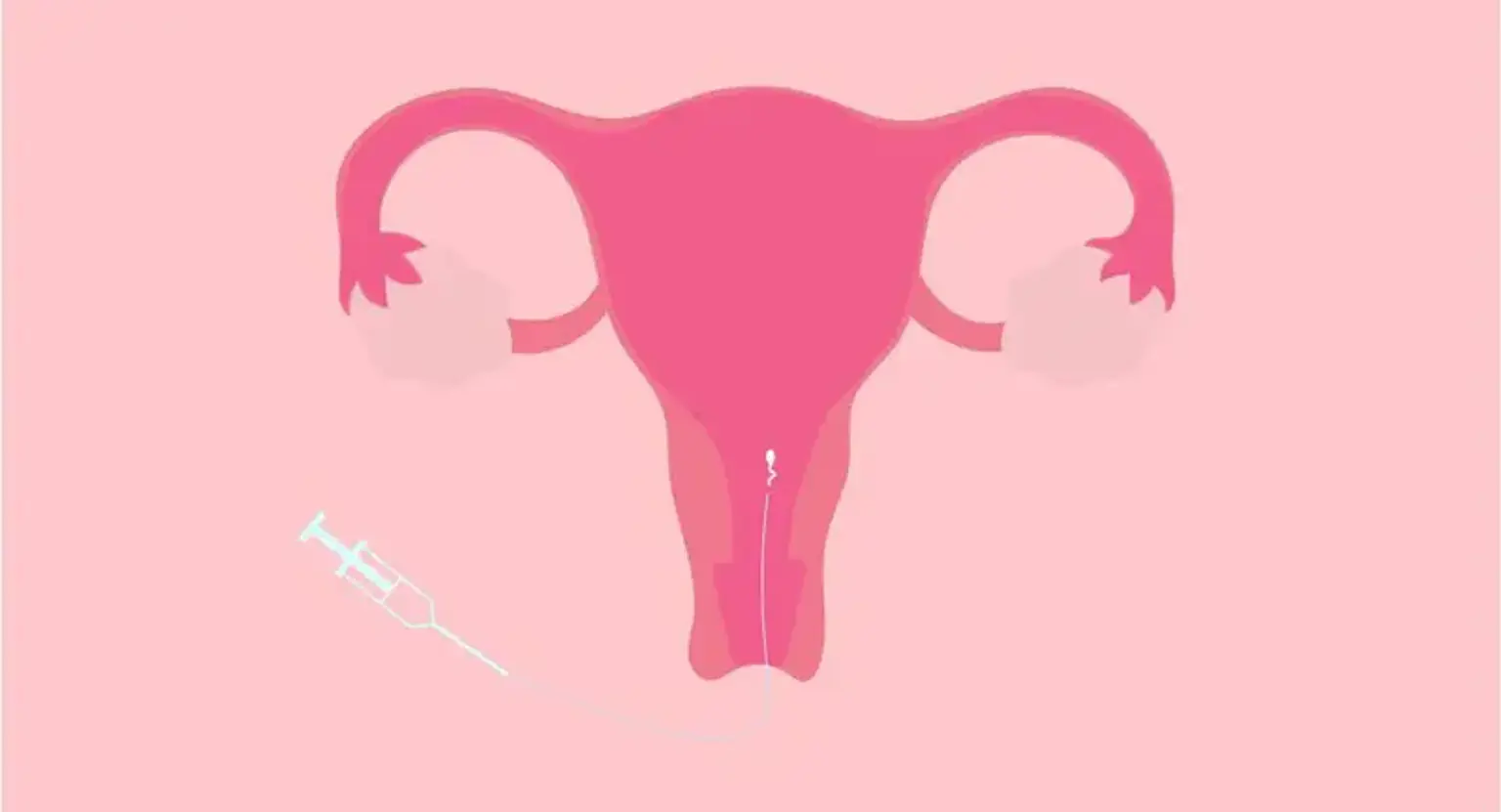
Sperm travels from the vagina through the cervix (the narrow, lower section of the womb), into the uterus, and up into one of the fallopian tubes when a woman conceives naturally. If sperm enters a tube shortly after the egg is released from the ovary (ovulation), the sperm and egg might meet and combine in the tube (fertilization).
The amount of sperm that enters the uterus is naturally limited by the cervix. This indicates that only a tiny fraction of the sperm in the ejaculate enters the fallopian tubes. Intrauterine insemination (IUI) is a process that puts sperm through the cervix and into a woman's uterus around the time of ovulation. This shortens the path to the fallopian tubes, increasing the likelihood that more sperm will reach the egg. This technique is intended to increase a woman's chances of becoming pregnant.