Mild IVF
Overview
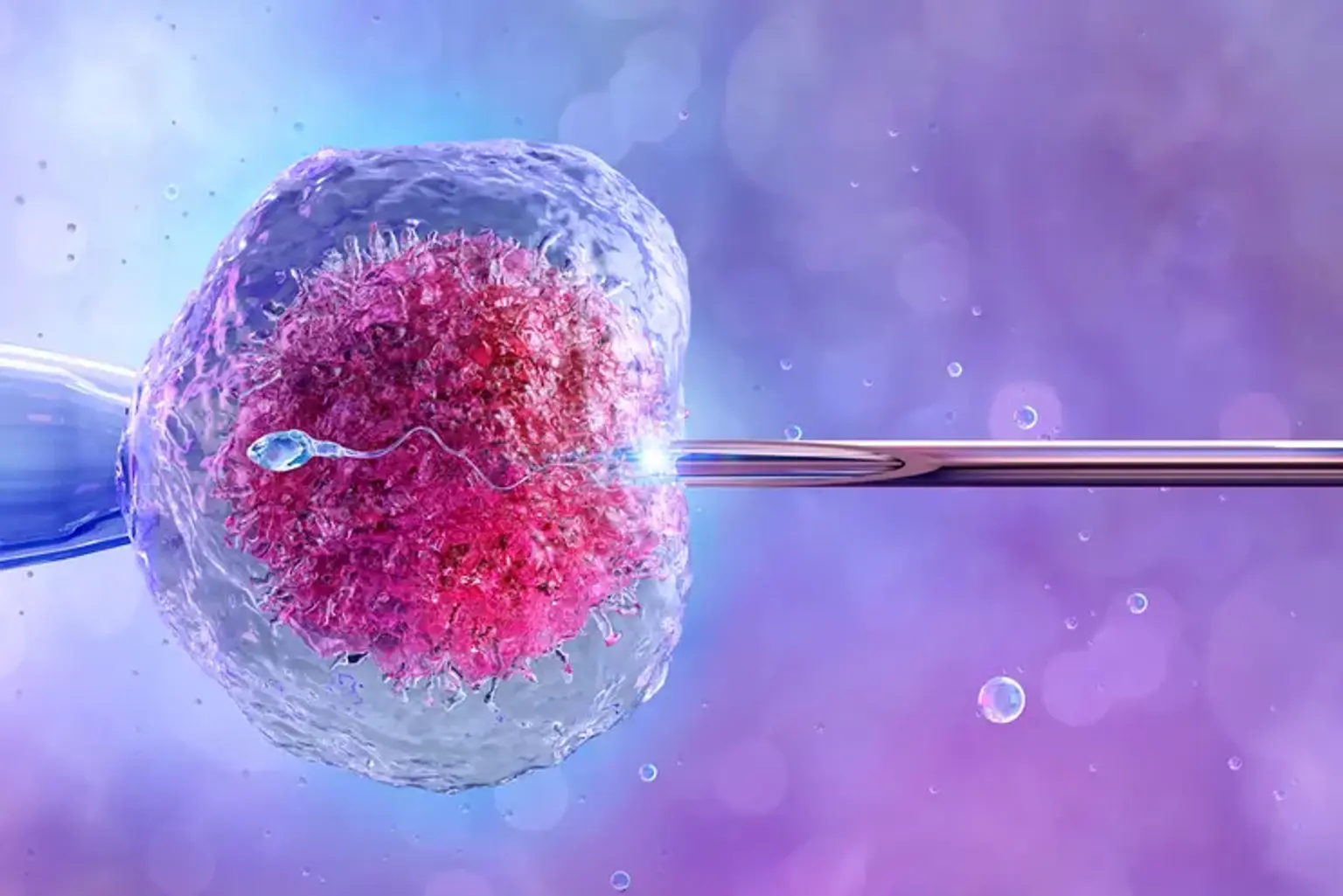
The procedures utilized during therapy for mild IVF often referred to as micro, mini or minimal stimulation IVF, are similar to those used for conventional IVF. You receive monitoring during the cycle, egg retrieval, laboratory fertilization of the egg and sperm, and embryo transfer, just like with IVF.
The amount of medication used to induce the ovaries to produce eggs differs. Mild IVF uses weaker drugs or lower doses of medications to create only a few eggs, as opposed to standard IVF, which tries to develop numerous eggs for retrieval. It can also be carried out without the use of any ovarian stimulants. Less fertility medication is used, which lowers the cost per cycle and lowers the risk of ovarian hyperstimulation syndrome (OHSS).