Minimally Invasive Valve Surgery
Overview
The tricuspid valve, pulmonary valve, mitral valve, and aortic valve are among the four valves in your heart that control blood flow. Regurgitation, in which blood leaks back through the valve in the wrong direction, can be caused by a damaged heart valve. It could also have stenosis, which causes the valve to not open as well as it should and obstruct blood flow. Additionally, the mitral valve doesn't shut tightly when it prolapses.
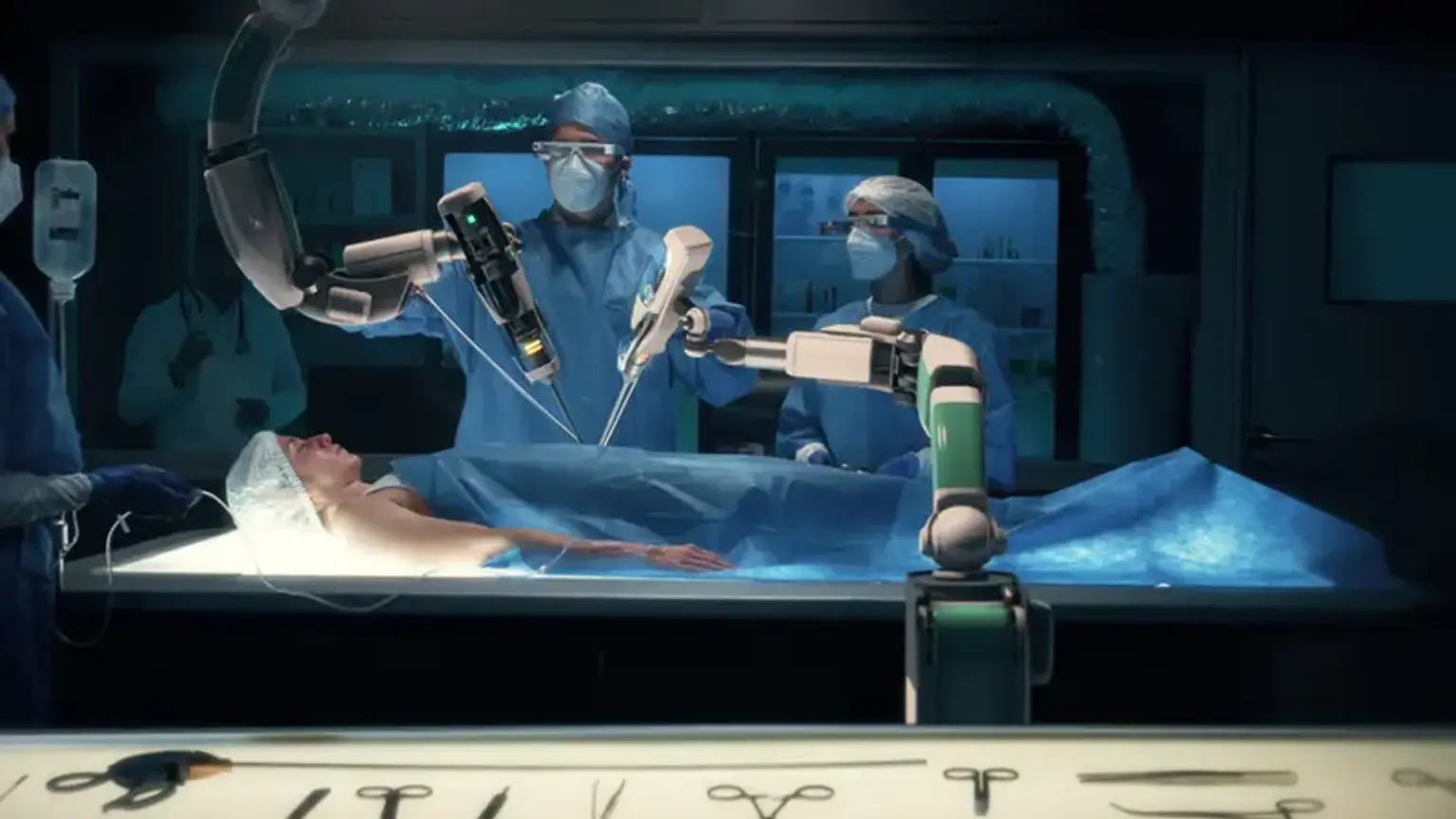
Your cardiologist might advise heart valve replacement or repair if you have a damaged heart valve. Your heart is medically stopped during valve surgery, and a heart-lung machine is used to oxygenate and circulate your blood. The damaged valve is removed by your surgeon, who then sews a replacement valve into place. Although a mechanical valve composed of plastic and metal is more frequently employed, the replacement valve may be taken from an organ donor.
Diseased valves can occasionally be repaired; for instance, if calcium deposits on the valve can be surgically removed, the valve may be reshaped to close more forcefully. Sometimes, if the valve hole is too large, sutures might be used to close it.