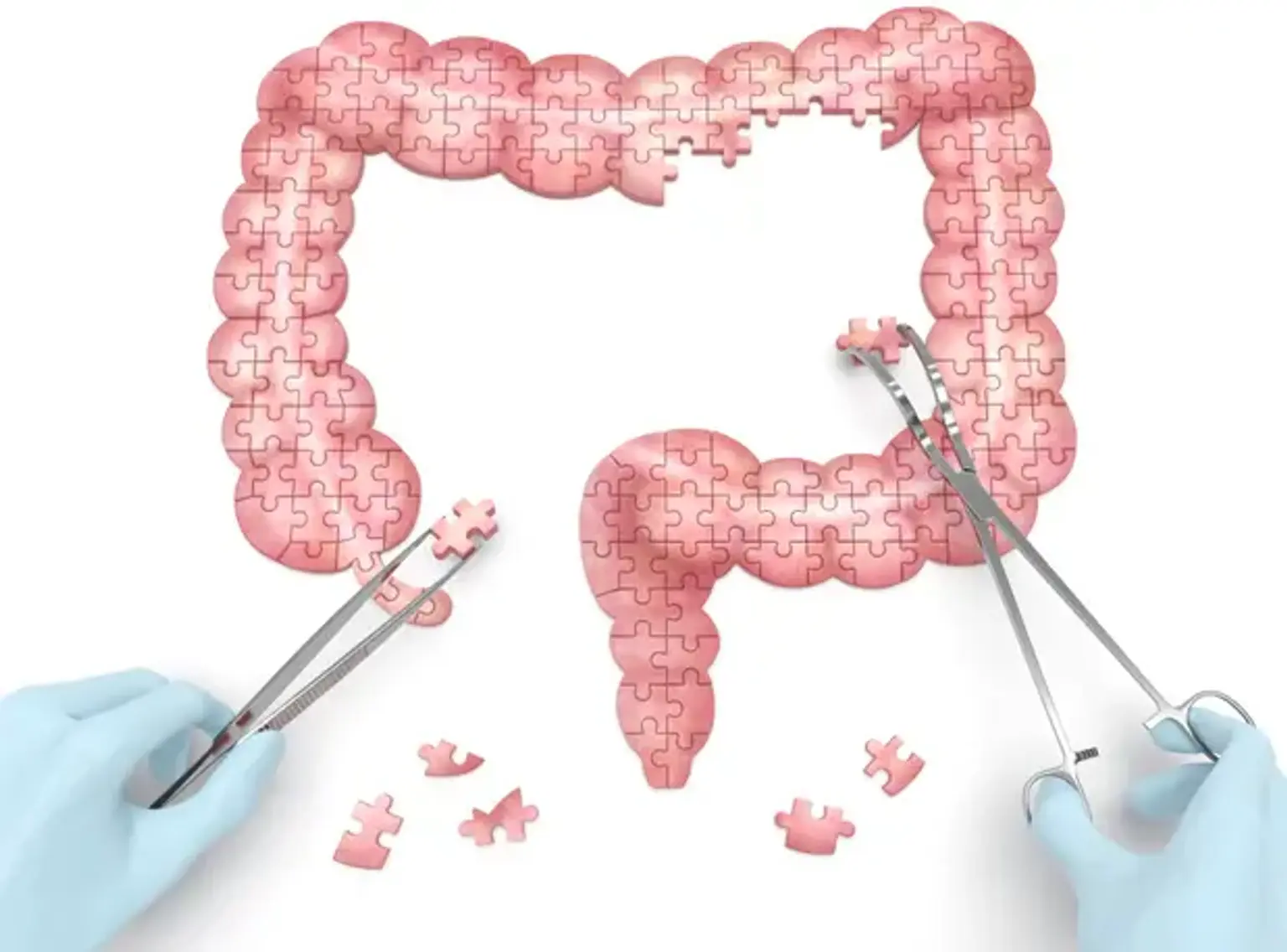
Partial Colectomy
Overview
There are several forms of colectomy, such as total colectomy (removal of the whole colon) and partial colectomy (Removal of part of the colon.). Total proctocolectomy (removal of the right or left side of the colon) (Removal of the colon and the rectum.).
A partial colectomy is a form of surgery used to treat disorders of the colon. Cancer, inflammatory illness, and diverticulitis are examples of them. A section of the colon is removed during the procedure. The colon is an extension of the big intestine. When treating cancer, the surgeon will frequently remove the cancerous portion of the colon. He or she will also remove a tiny portion on either side of the cancerous region. He or she will also remove several lymph nodes nearby. The colon's remaining pieces are then joined together. Alternatively, an opening to the exterior of the body (stoma) is formed. This is known as a colostomy.