Perilymph fistula (PLF)
What is Perilymph fistula?
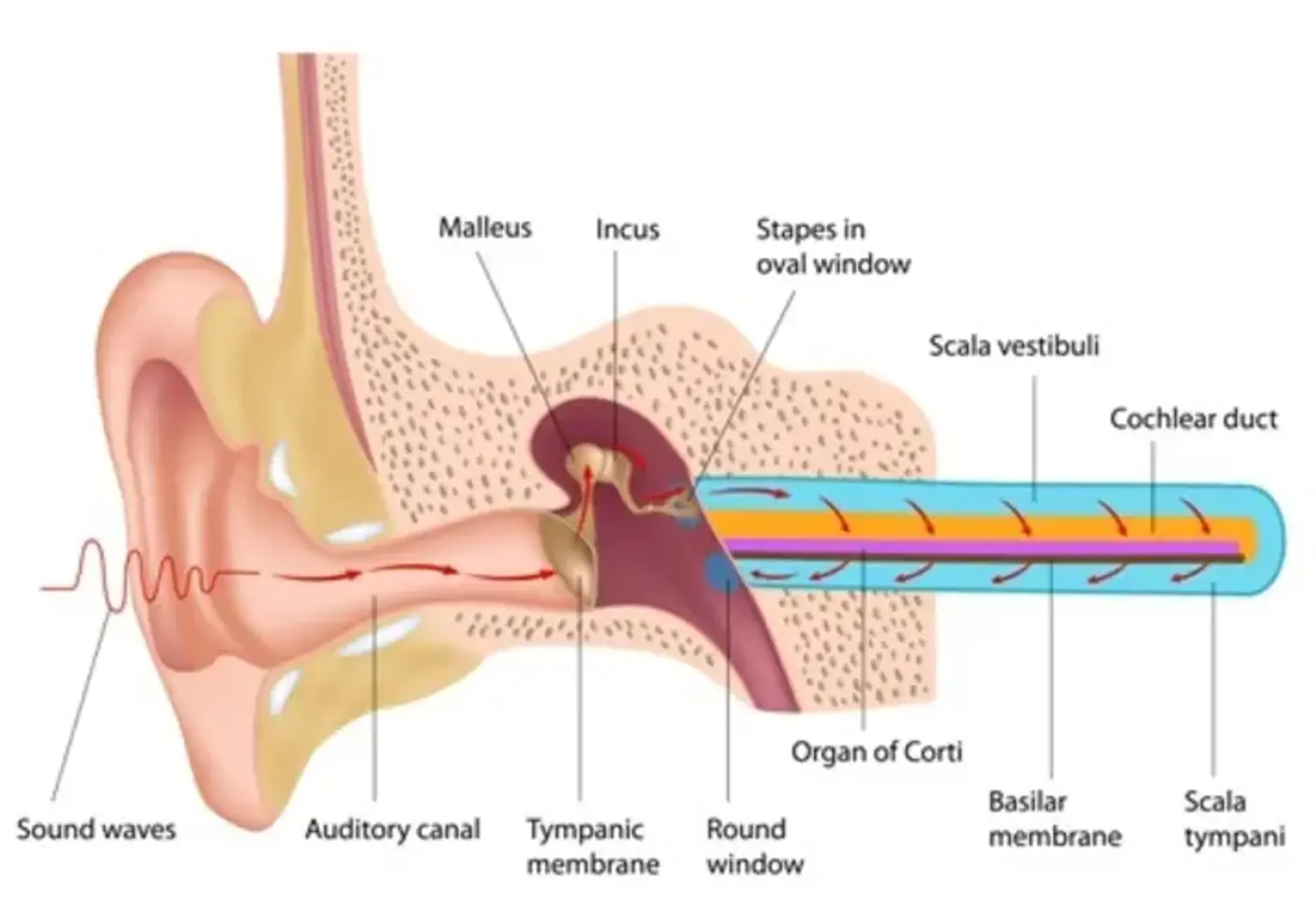
A perilymph fistula (PLF) is a break or defect in the membranes that divide the middle ear from the inner ear's perilymphatic region. Fluid may drain into the middle ear as a result of the tear. It can also induce pressure changes in the middle ear, which can affect the inner ear and generate abnormal symptoms.
A perilymph fistula (PLF) is a hole or tear in one of the membranes that separate your middle ear from your inner ear. Your middle ear contains air, whereas your inner ear contains fluid (perilymph). Membranes divide these two locations inside your ear. Perilymphatic fluid can leak from your inner ear into your middle ear if the membranes break. The pressure fluctuations that follow might cause balance and hearing issues.