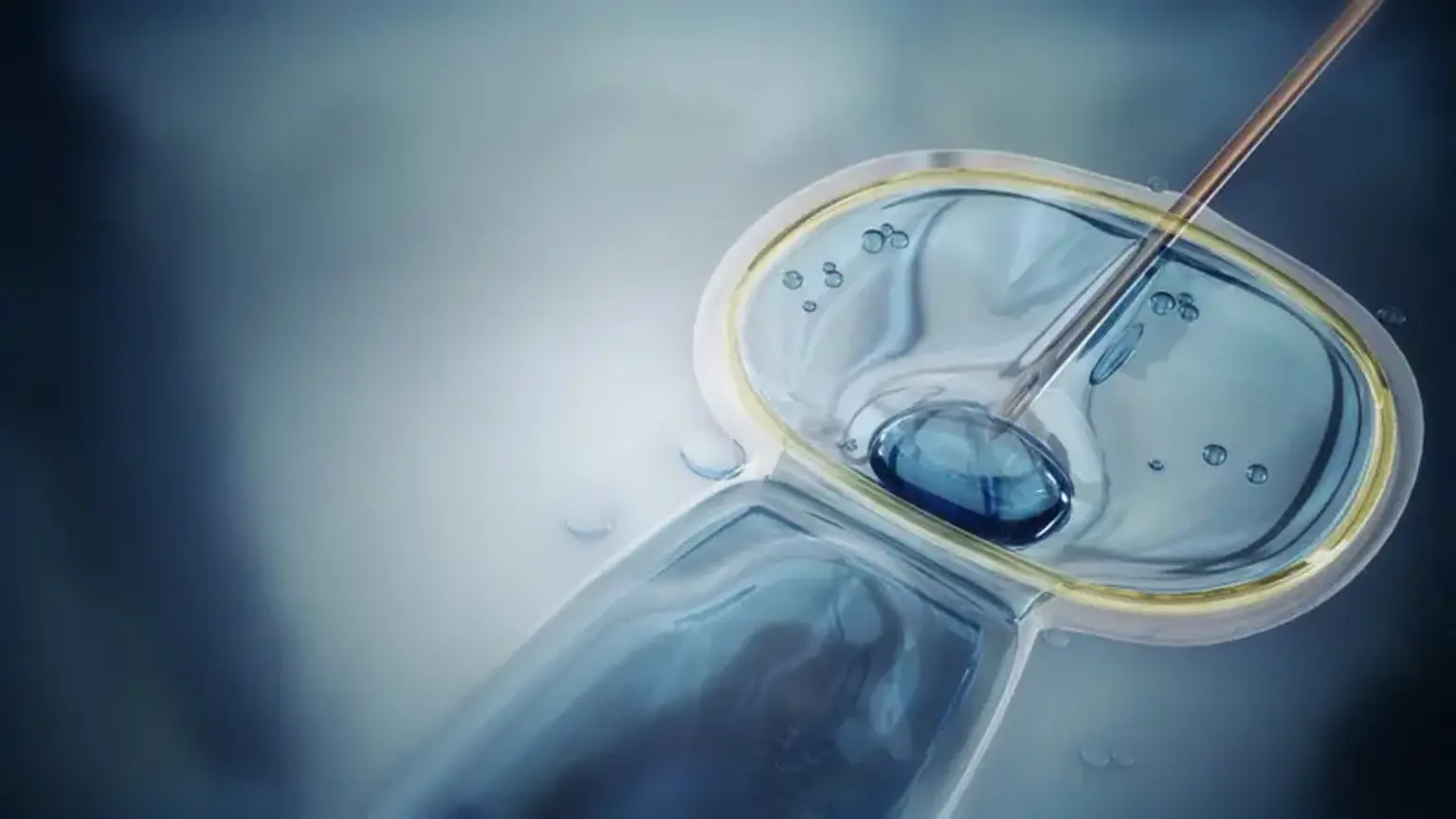
Physiological intracytoplasmic sperm injection (PICSI)
Overview
About 20 % of patients are diagnosed infertile without specific causes. Various techniques and procedures have rapidly emerged over 3 decades in assisted reproduction, but the success rate remains alike. In totting up, petite ratios of couples do not succeed in conceiving despite multiple in vitro fertilization (IVF) or ICSI Intracytoplasmic sperm injection procedures.