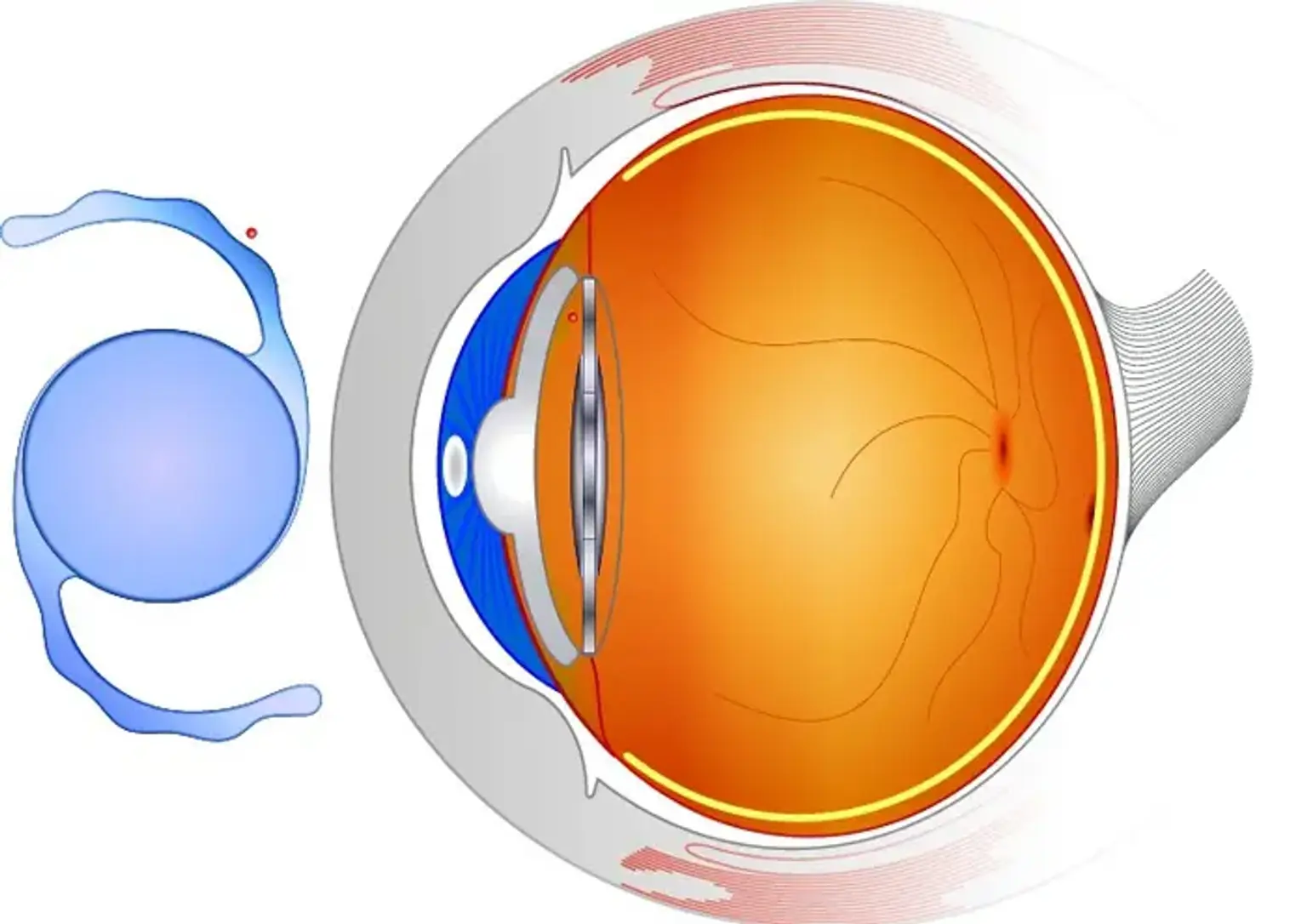
Phakic Intraocular Lens (PIOL) Implantation
Overview
Myopia is a major public health concern across the world. People nowadays spend an increasing amount of time on computers and mobile phones. As a result, the number of patients suffering from myopia has increased. Because wearing thick glasses is not always comfortable, corneal laser refractive surgery and phakic intraocular lens (pIOL) implantation are commonly used to treat myopia.