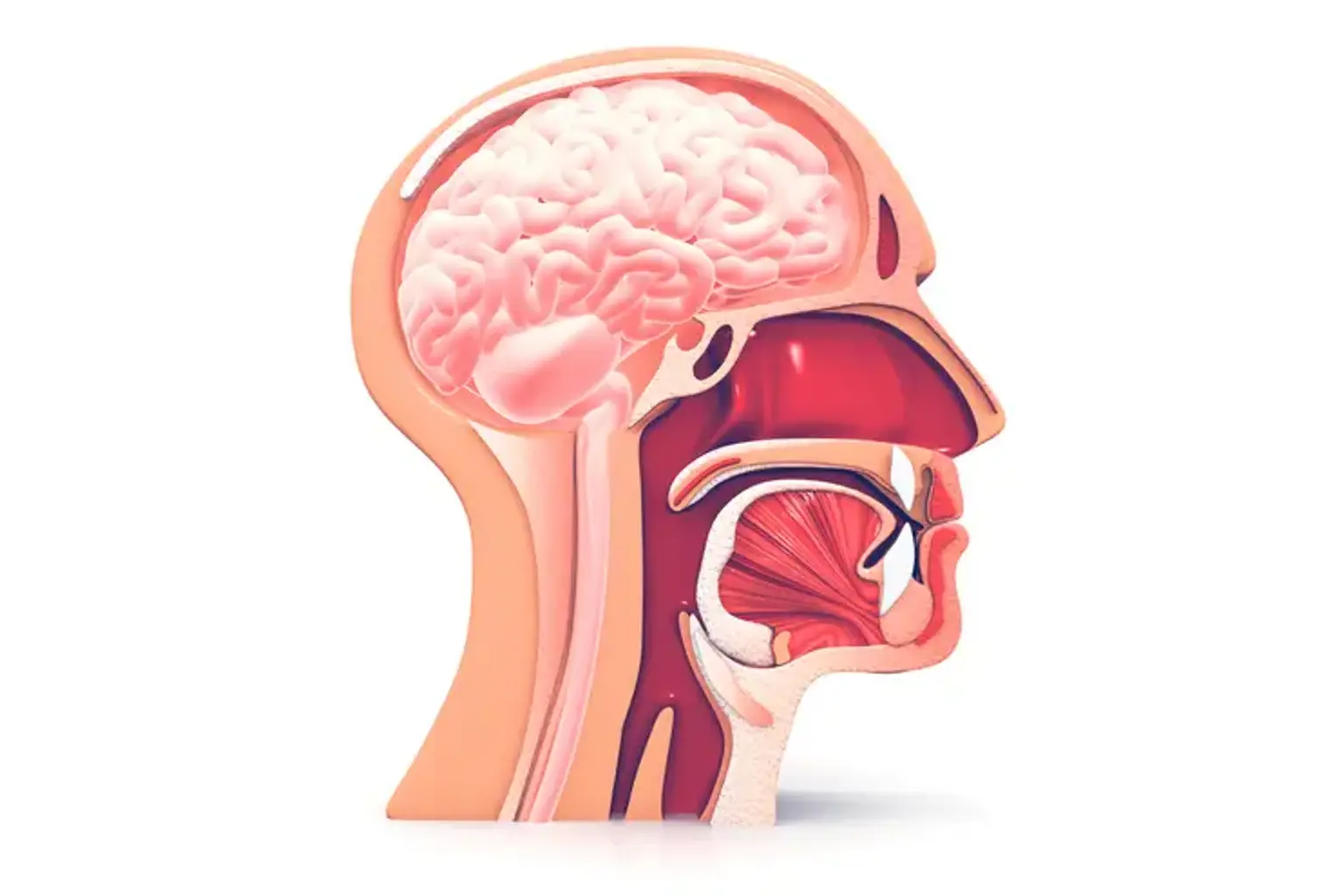
Pituitary Surgery
To remove pituitary tumors while preserving as many of the healthy gland's tissues as feasible, many surgeons perform pituitary surgery. This makes it possible for the gland to continue secreting the appropriate amount of hormones, which are essential for carrying out various body activities. When pituitary tumors cause Cushing's disease, acromegaly, secondary hyperthyroidism, hypopituitarism, visual issues, or malignant tumors, surgery is frequently the initial course of treatment. Rare emergencies such as the destruction or hemorrhage into the pituitary gland may also call for surgery.