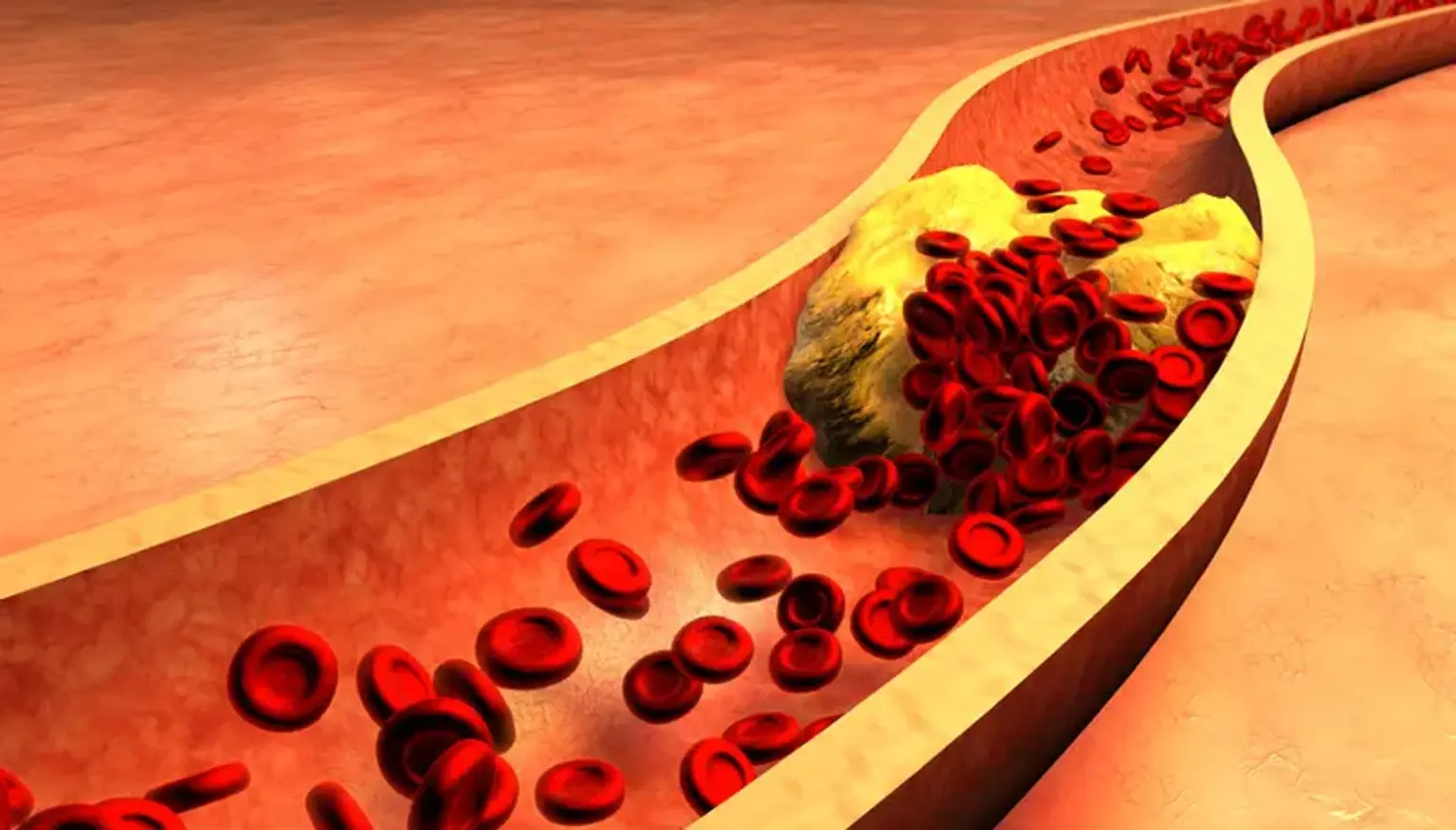
Chronic Occlusion Coronary Artery (CTO)
According to angiographic evidence, a chronic occlusion coronary artery or chronic total occlusion of the coronary artery (CTO) is when a coronary artery is completely blocked for a length of time more than or equivalent to three months. The TIMI (thrombolysis in myocardial infarction) flow grading method provides the levels of coronary blood flow obtained during coronary angiography with a scoring classification from 0 to 3. The following is the TIMI flow grading system:
- TIMI 0 flow (no perfusion-complete occlusion). There is no forward flow after a coronary blockage.
- TIMI 1 flow (penetration without perfusion). A slight forward flow beyond the blockage with an incomplete filling of the distal coronary bed.
- TIMI 2 flow (partial reperfusion). Delayed forward flow with a full filling of the distal coronary bed.
- TIMI 3 flow (full perfusion). The distal coronary bed is filled with normal coronary blood flow.
According to angiographic evidence, a true chronic occlusion coronary artery is defined as a coronary artery that is completely blocked with zero TIMI flow; in contrast, a functional CTO is described as a coronary artery that is significantly stenotic but has TIMI 1 flow over a while longer than or equivalent to 3 months. Furthermore, in the absence of serial angiograms, it can be challenging to identify the exact time frame during which a chronic occlusion coronary artery lesion was present, Therefore, the date of the event that produced the occlusion is primarily estimated based on clinical data that is now accessible, such as a recent myocardial infarction or a sudden shift in anginal symptoms with ECG abnormalities corresponding with the location of the occlusion. The duration of the CTO cannot be accurately estimated in many patients, though.