Gastrointestinal Robotic Surgery
There have been two major developments in the treatment of gastrointestinal cancer in the last 20 years. The evidence-based standardization of anticancer medication treatment, which was based on the outcomes of many research (including randomized controlled trials) conducted around the world, is one example of a breakthrough. The spread of minimally invasive surgery, such as laparoscopic and thoracoscopic surgery, is another breakthrough. Endoscopic surgery, such as laparoscopic surgery and thoracoscopic surgery, is increasingly commonly utilized for gastrointestinal cancers, including esophageal cancer, stomach cancer, hepatopancreatobiliary cancer, and colorectal cancer. However, unlike the above-mentioned standard of anticancer drug treatment, the expansion of minimally invasive surgery is not supported by solid evidence. Surgical techniques and skills utilized in gastrointestinal cancer surgery vary depending on the facility and surgeon. As a result, unlike the outcomes of anticancer drug therapies, it is extremely difficult to compare outcomes such as surgery's curability and complications.
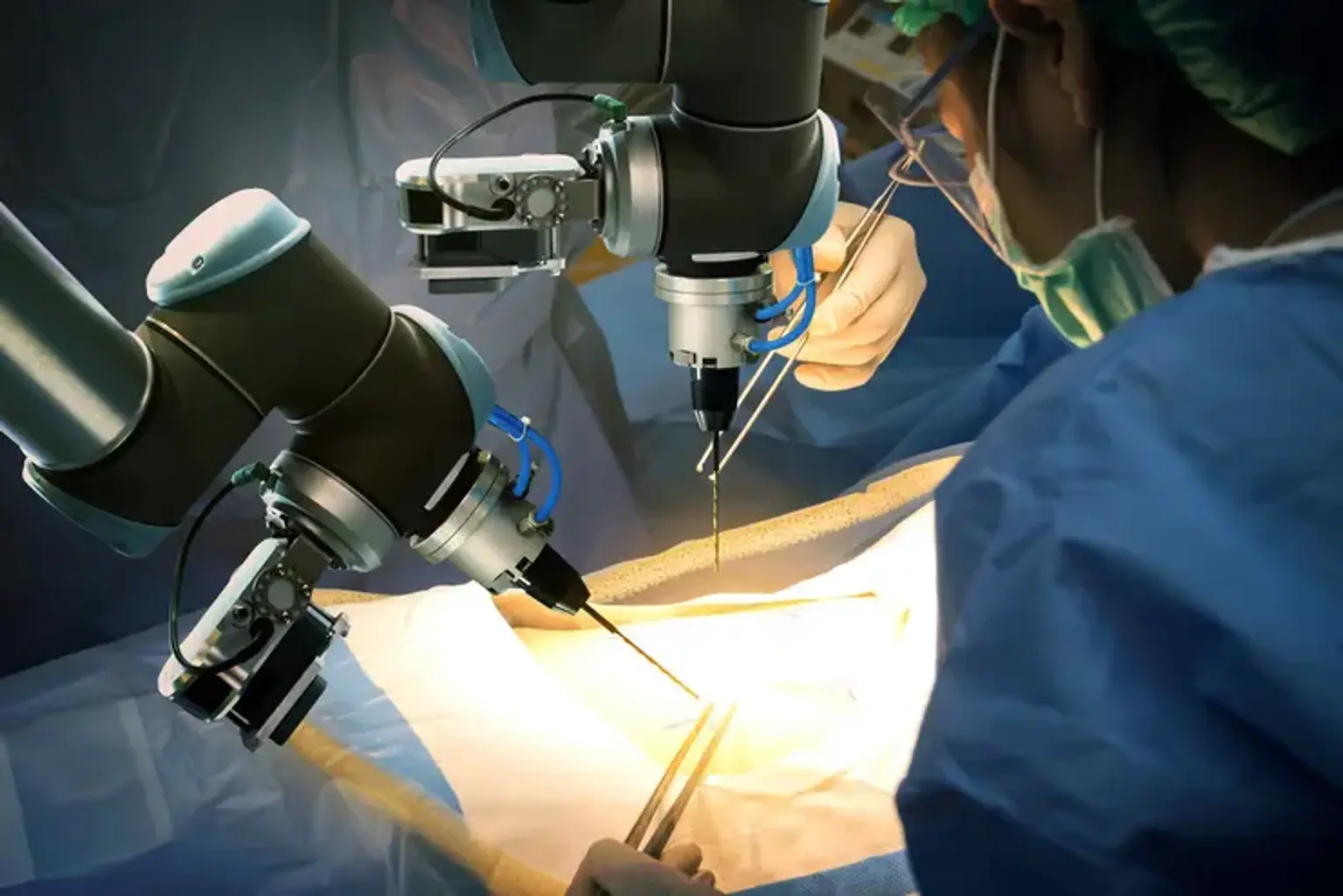
Robotic surgery in gastrointestinal surgery is becoming more popular as one of the most promising types of minimally invasive procedures. A robot-assisted surgery system is used to perform robotic surgery in the area of gastrointestinal diseases.