Microsurgical Hepatic Artery Reconstruction
After providing supportive care to the patient, liver transplantation is the only effective treatment for acute or chronic liver failure. Shorter survival time (which is regarded as less than a year) and unsatisfactory life quality owing to liver disease are the two indications for liver transplantation that are widely accepted by the medical world. Starzl carried out the first successful liver transplant in the 1960s. The importance and popularity of liver transplants are growing daily and are now conducted in two categories: cadaveric donor liver transplantation (CDLT) and living donor liver transplantation (LDLT). Strong kinship ties, insufficient liver donors, and liver procurement issues have all contributed to higher LDLT rates than CDLT. Since it was first published in the 1980s, thousands of LDLT procedures have been carried out in numerous hospitals all over the world.
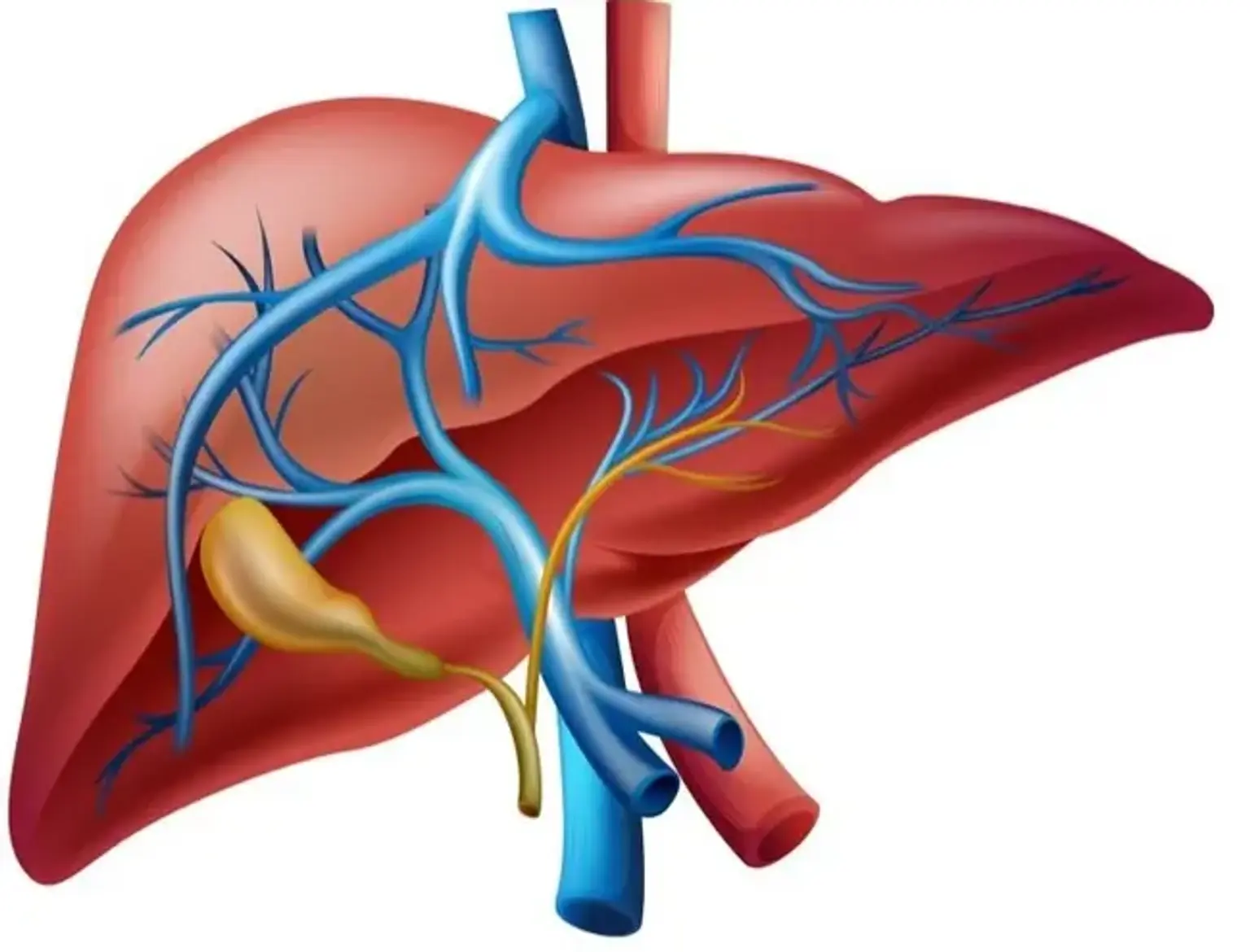
In CDLT, the recipient's hepatic artery system is anastomosed to the hepatic artery system that was removed at the aortic level. Therefore, since this is a gross vascular process, no microsurgical methods are needed. However, in LDLT, the hepatic lobule and its associated hepatic artery are transferred. Due to the procedure's small diameter, microsurgical reconstruction methods and tools are required. The hepatic artery and the portal vein each give blood to the liver separately. As a result, blood enters the parenchyma through both of them, but the biliary tract has no connection to portal circulation. Because of this, the outcome of the surgery and the patient's survival is directly impacted by the reconstruction success. Otherwise, death is the consequence of the situation. While other medical specialties with skills in microsurgery have conducted hepatic artery reconstruction, it is normal practice for plastic surgeons to perform it in many hospitals across the world.