Shoulder Replacement
Overview
Although shoulder joint replacement is less prevalent than knee or hip replacement, it is as effective in alleviating joint discomfort.
Shoulder replacement surgery was initially used to treat serious shoulder fractures in the 1950s in the United States. Over time, shoulder joint replacement has grown to be utilized for a variety of additional painful shoulder disorders, such as various kinds of arthritis.
According to the Agency for Healthcare Research and Quality, around 53,000 people in the United States receive shoulder replacement surgery each year. This contrasts to over 900,000 Americans who get knee and hip replacement surgery each year.
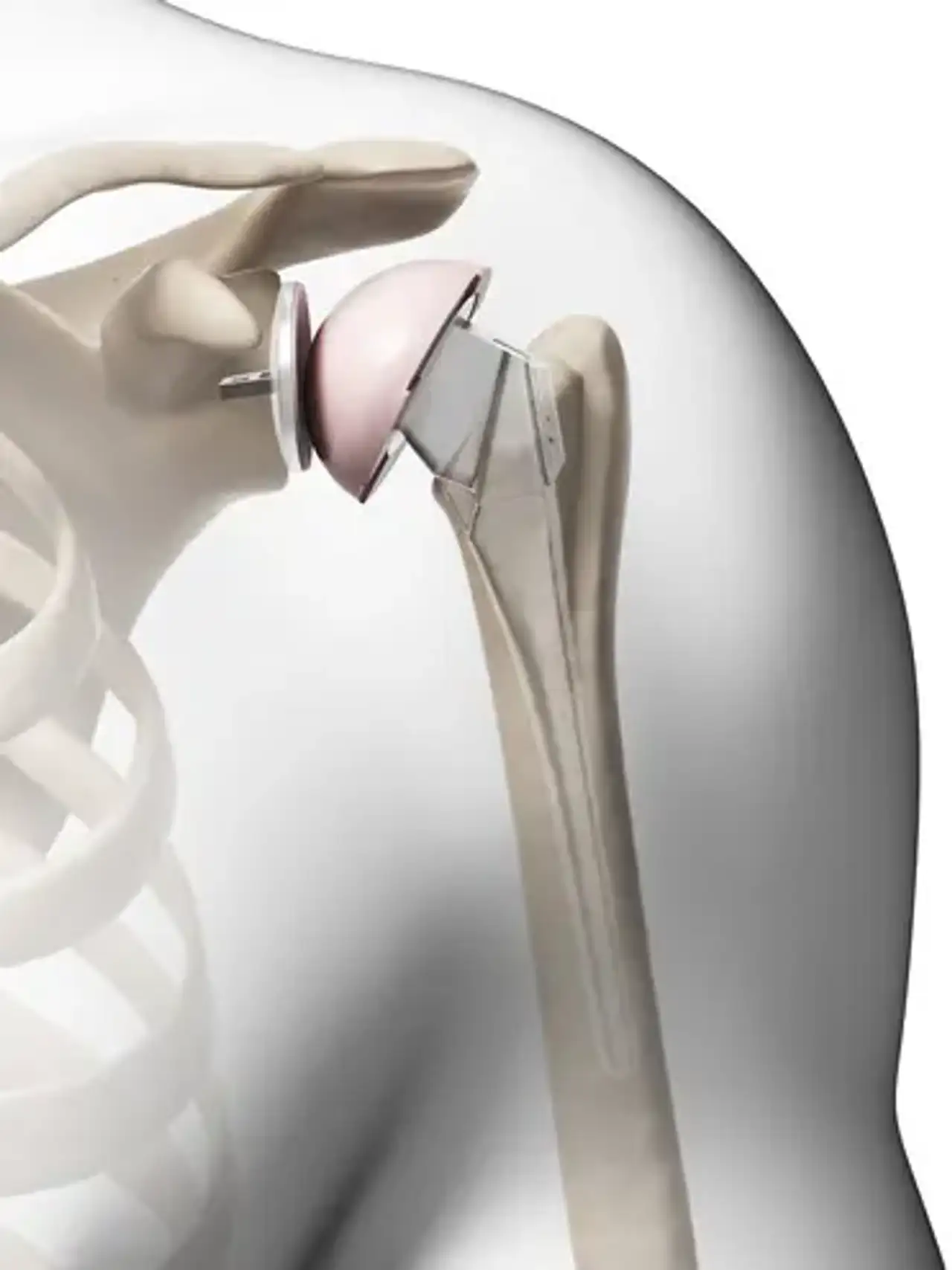
Shoulder replacement is a surgical technique in which a prosthetic implant replaces all or part of the glenohumeral joint. Joint replacement surgery is often performed to ease arthritic discomfort or to repair significant physical joint deterioration.
Shoulder replacement surgery is an option for treating severe shoulder arthritis like those with significant rheumatoid arthritis. Arthritis is a disorder that affects the joint cartilage. The protective coating between the bones is lost when the cartilage lining goes away. Painful bone-on-bone arthritis occurs as a result of this. Severe shoulder arthritis is extremely uncomfortable and might limit movement. While certain drugs and lifestyle changes may help, there may come a time when surgical treatment is required.
Anatomy of Shoulder joint
The upper arm bone (humerus), the shoulder blade (scapula), and the collarbone comprise your shoulder joint. The shoulder is a ball-and-socket joint, which means it has two parts: the ball and the socket. Your upper arm bone's ball, or head, fits into a shallow socket in your shoulder blade. The glenoid is the name given to this socket.
The surfaces of the bones that come into contact with each other are coated with articular cartilage, a smooth material that protects the bones and allows them to move freely. All remaining surfaces inside the shoulder joint are covered by a thin, smooth tissue called synovial membrane. In a healthy shoulder, this membrane produces a little quantity of fluid that lubricates the cartilage and almost eliminates shoulder friction.
Stability and support are provided by the muscles and tendons that surround the shoulder.
All of these components allow the shoulder to spin more freely than any other joint in the body.
What Are Prostheses Made of?
A metal ball is utilized to replace the humeral ball, which is constructed of a particular type of stainless steel and is coupled to a titanium stem to maintain the ball attached to your arm, while a polyethylene cup replaces the glenoid socket.
When Shoulder Joint Replacement Is Needed?
A variety of disorders can cause shoulder discomfort and impairment, prompting patients to seek shoulder joint replacement surgery.
- Osteoarthritis (Degenerative Joint Disease):
Osteoarthritis is a kind of arthritis caused by age-related wear and strain. It mainly affects persons over the age of 50, although it can also affect younger people. The cartilage that cushions the shoulder bones shrinks and wears away. The bones then grate against one other. The shoulder joint gradually stiffens and becomes uncomfortable over time.
Unfortunately, there is no way to prevent osteoarthritis from developing. It is a common indication for shoulder replacement surgery.
- Rheumatoid Arthritis:
The synovial membrane that covers the joint becomes inflamed and swollen in this condition. Chronic inflammation can harm cartilage, resulting in cartilage loss, discomfort, and stiffness. Rheumatoid arthritis is the most frequent kind of an inflammatory arthritis group of disorders.
- Post-traumatic Arthritis:
This can happen after a significant shoulder injury. Fractures of the shoulder bones or rips of the shoulder tendons or ligaments can cause articular cartilage degradation over time. This results in shoulder discomfort and a reduction in shoulder function.
- Rotator Cuff Tear Arthropathy:
Cuff tear arthropathy can occur in a patient who has a substantial, long-standing rotator cuff tear. The alterations in the shoulder joint caused by the rotator cuff rupture may lead to arthritis and cartilage loss in this disorder.
- Avascular Necrosis (Osteonecrosis):
Avascular necrosis, also known as osteonecrosis, is a painful disorder caused by a disruption in the blood flow to the bone. Because bone cells die in the absence of a blood supply, osteonecrosis can eventually destroy the shoulder joint and contribute to arthritis. Chronic steroid usage, deep sea diving, severe shoulder fractures, sickle cell disease, and excessive alcohol use are all risk factors for avascular necrosis.
- Severe Fractures:
Another typical reason for shoulder replacement is a serious fracture of the shoulder. When the head of the upper arm bone is fractured, it may be difficult for a doctor to reattach the shards of bone. Furthermore, the blood flow to the bone fragments may be disrupted. A shoulder replacement may be recommended in this scenario by a surgeon. Severe shoulder fractures are more common in elderly people with osteoporosis.
- Failed Previous Shoulder Replacement Surgery:
Although rare, some shoulder replacements fail due to implant loosening, wear, infection, or dislocation. When this happens, a second joint replacement procedure, known as a revision surgery, may be required.
Types of Shoulder Replacements
Shoulder replacement surgery is a very complex procedure. It should be carried out by a surgical team having prior expertise with this technique.
Shoulder replacements come in a variety of styles. Before making any judgments, your surgeon will thoroughly assess your circumstances. They will consult with you to determine which sort of replacement will best satisfy your medical needs. Do not be afraid to inquire about the sort of implant that will be utilized in your case and why that decision is best for you.
1. Total Shoulder Replacement:
A highly polished metal ball coupled to a stem and a plastic socket replaces the arthritic joint surfaces in a conventional complete shoulder replacement.
These components are available in a variety of sizes. They can be glued or pressed into the bone. If the bone quality is good, your surgeon may opt for a non-cemented (press-fit) humeral component. The humeral component may be implanted with bone cement if the bone is soft. In most situations, bone cement is used to implant an all-plastic glenoid (socket) component.
Implantation of a glenoid component is not advised if:
- The glenoid has good cartilage.
- The glenoid bone is severely deficient.
- The rotator cuff tendons are irreparably torn.
Patients with bone-on-bone osteoarthritis and intact rotator cuff tendons are generally good candidates for conventional total shoulder replacement.
2. Stemmed Hemiarthroplasty
Depending on the state of your shoulder, your surgeon may merely replace the ball. A hemiarthroplasty is the medical term for this treatment. The surgeon replaces the head of the humerus with a metal ball and stem, identical to the component used in a total shoulder replacement, in a typical hemiarthroplasty. This is referred to as a stemmed hemiarthroplasty.
When the humeral head is badly shattered but the socket is normal, some surgeons propose hemiarthroplasty. Other reasons for a hemiarthroplasty are as follows:
- Arthritis that involves only the head of the humerus, with a glenoid that has a healthy and intact cartilage surface.
- Shoulders with severely weakened bone in the glenoid.
- Some shoulders with severely torn rotator cuff tendons and arthritis.
- Sometimes, surgeons make the decision between a total shoulder replacement and a hemiarthroplasty in the operating room at the time of the surgery.
- Studies show that patients with osteoarthritis get better pain relief from total shoulder arthroplasty than from hemiarthroplasty.
3. Resurfacing Hemiarthroplasty
Resurfacing hemiarthroplasty includes replacing just the humeral head's joint surface with a cap-like prosthesis that lacks a stem. With its bone-preserving benefit, it provides an option to the traditional stemmed shoulder replacement for patients with shoulder arthritis.
Resurfacing hemiarthroplasty may be an option for you if:
- The glenoid still has an intact cartilage surface.
- There has been no fresh fracture of the humeral neck or head.
- There is a desire to preserve humeral bone.
Resurfacing hemiarthroplasty eliminates the hazards of component wear and loosening that might arise with traditional complete shoulder replacements in patients who are young or extremely active. Because of its more conservative nature, resurfacing hemiarthroplasty may be easier to convert to complete shoulder replacement in the future if necessary.
4. Reverse Total Shoulder Replacement
Another type of shoulder replacement is called reverse total shoulder replacement. Reverse total shoulder replacement is used for people who have:
- Completely torn rotator cuffs with severe arm weakness
- The effects of severe arthritis and rotator cuff tearing (cuff tear arthropathy)
- Had a previous shoulder replacement that failed
For some people, a traditional complete shoulder replacement may still cause discomfort. They can also be unable to raise their arm over a 90-degree angle. Being unable to move your arm away from your side can be quite painful.
The socket and metal ball are switched in reverse complete shoulder replacement: a metal ball is connected to the shoulder bone, and a plastic socket is affixed to the upper arm bone. This permits the patient to lift the arm using the deltoid muscle rather than the damaged rotator cuff.
Preparing for Surgery
- Medical Evaluation:
If you elect to have shoulder replacement surgery, your orthopaedic surgeon may request that you arrange a comprehensive physical examination with your primary care physician several weeks before the procedure. This is required to ensure that you are in good enough health to have surgery and recover fully. Before surgery, many patients with chronic medical issues, such as heart disease, must be assessed by a specialist, such as a cardiologist.
- Medications:
Make sure to inform your orthopaedic surgeon about any drugs you are taking. Some drugs may need to be discontinued prior to surgery. Over-the-counter medications, for example, may cause severe bleeding and should be discontinued two weeks before surgery:
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen
- Most arthritis medications
- If you take blood thinners, either your primary care doctor or cardiologist will advise you about stopping these medications before surgery.
- Home Planning:
Making minor improvements to your house before surgery might help you recover more quickly.
It will be difficult to reach high shelves and cupboards for several weeks following your operation. Before your procedure, walk around your house and put any objects you might need later on low shelves.
When you get home from the hospital, you will want assistance with daily duties such as dressing, bathing, cooking, and laundry for a few weeks. If you will not have any help at home soon following surgery, you may require a brief stay in a rehabilitation center until you are more self-sufficient.
The Day of Surgery
Before Your Operation:
When you go to the hospital for your procedure, wear loose-fitting pants and a button-front shirt. You will be wearing a sling and will have restricted use of your arm following surgery.
On the day of your operation, you will almost certainly be admitted to the hospital. After admission, you will be transported to the preoperative preparation area and meet with an anesthetic department doctor.
The sort of anesthetic to be used will be discussed by you, your anesthesiologist, and your surgeon. You may be given a general anesthetic (in which you are unconscious throughout the procedure), a regional anesthetic (in which you are awake but have no feeling around the surgical area), or a mix of the two.
Surgical Procedure:
It normally takes around 2 hours to replace your shoulder joint with an artificial device.
Following surgery, you will be sent to the recovery room, where you will remain for many hours while your anesthetic recovery is monitored. You will be escorted to your hospital room after you have awakened.
What Happens After Your Surgery?
To avoid infection, your medical team will administer numerous doses of antibiotics. The day following surgery, the majority of patients are able to consume solid meals and get out of bed. You will most likely be allowed to leave the hospital on the first, second, or third day following surgery.
- Pain Management:
You will have some discomfort following surgery. This is a normal component of the recovery process. Your doctor and nurses will attempt to lessen your discomfort, which will allow you to recover from surgery more quickly.
Medications are frequently recommended for short-term pain management following surgery. Opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and local anesthetics are just a few of the medications available to aid with pain management. Your doctor may prescribe a combination of these drugs to alleviate pain and reduce the need for opioids.
Be aware that, while opioids can help with pain relief after surgery, they are a narcotic and can be addicted. Opioid addiction and overdose have become major public health concerns in the United States. It is critical to only use opioids as prescribed by your doctor and to discontinue them as soon as your pain begins to improve. Consult your doctor if your pain does not improve within a few days following your procedure.
Pain management is a critical component of your recovery. You will begin physical therapy immediately after surgery, and as you experience less pain, you will be able to move more rapidly and regain strength. If postoperative discomfort becomes an issue, consult your doctor.
- Rehabilitation:
A well-planned rehabilitation program is essential to the success of a shoulder replacement. Gentle physical rehabilitation is generally started immediately after the procedure. Your surgeon or physical therapist will give you a home workout routine to help you strengthen and stretch your shoulder.
Home Going Instructions
- Check the incision on a regular basis for any signs of edema or discharge.
- Maintain the dressing's integrity. Because your dressing is sealed, you will be able to bathe and shower. Allow the water to drip over it and then pat it dry. At your first follow-up session, your dressing will be removed.
- You will be offered a return appointment 10 to 14 days later to remove your dressing, as well as a prescription for pain medication, at the time of release.
- Your healthcare professional will advise you on particular precautions and activity limitations.
- Drive according to your healthcare provider's instructions. You will, however, need to have a driver ready to take you home after you are discharged.
- For the first two to four weeks, avoid lifting anything heavier than a glass of water.
- For the next two months, avoid carrying large things.
- Return to vigorous arm movement within the limitations of pain.
- Continue the activities you've been doing at home, as directed by your physical therapist and other healthcare specialists. Take cautious not to overdo it!
- Do not use your operating arm to help you get out of a bed or chair.
- Don't undertake any hard lifting on a regular basis. Play no contact sports.
- Avoid placing your arm in any “extreme position” for the first six weeks after surgery. An example is to not stretch your arm straight out to the side or behind your back.
Complications of The Procedure
Your orthopaedic surgeon will describe the possible risks and consequences of shoulder joint replacement surgery, including those connected to the operation itself as well as those that can develop thereafter.
When issues arise, the majority of them are effectively treated. The following are examples of potential difficulties:
- Infection: Infection is a risk with every operation. Infection can arise in the incision or deep surrounding the prosthesis after shoulder joint replacement. It might happen while you're in the hospital or after you leave. It might happen years later. Antibiotics are commonly used to treat minor infections in the wound area. Major or deep infections may necessitate further surgery and the removal of the prosthesis. Any infection in your body has the potential to spread to your joint replacement.
- Prosthesis Problems: Despite advances in prosthetic designs and materials, as well as surgical methods, the prosthesis may wear out and the components may become loose. A shoulder replacement's components may potentially dislocate. Excessive wear, loosening, or dislocation may necessitate further surgery (revision procedure).
- Nerve damage: Nerves near the joint replacement may be injured during surgery, though this is an uncommon complication. These nerve injuries frequently heal and may totally recover over time.
Conclusion
A shoulder replacement is a surgical treatment that replaces damaged portions of the shoulder joint with artificial components known as prostheses in an attempt to eliminate the source of pain and dysfunction.
A ball-and-socket joint, the shoulder is a ball-and-socket joint. The upper arm bone's spherical head (ball) fits into a shallow socket in the shoulder. Joint damage can result in pain, weakness, and stiffness.
Osteoarthritis, rotator cuff tear arthropathy, avascular necrosis, and rheumatoid arthritis are the most prevalent causes for shoulder replacement surgery. The operation is designed to reduce your discomfort, enhance your strength, expand your range of motion, and allow you to utilize your shoulder and arm again.
Shoulder implants are available in a variety of forms and sizes. Partial and complete replacement are available, with anatomic or reverse implants.
Although it is uncommon, it is conceivable that shoulder replacement surgery will not alleviate or eliminate your discomfort entirely. The procedure may not completely restore the joint's mobility or strength. Another operation may be required in some circumstances. Dislocation, fracture, implant loosening, rotator cuff failure, nerve damage, blood clots, and infection are all possible consequences of shoulder replacement surgery.