Avascular Necrosis
Overview
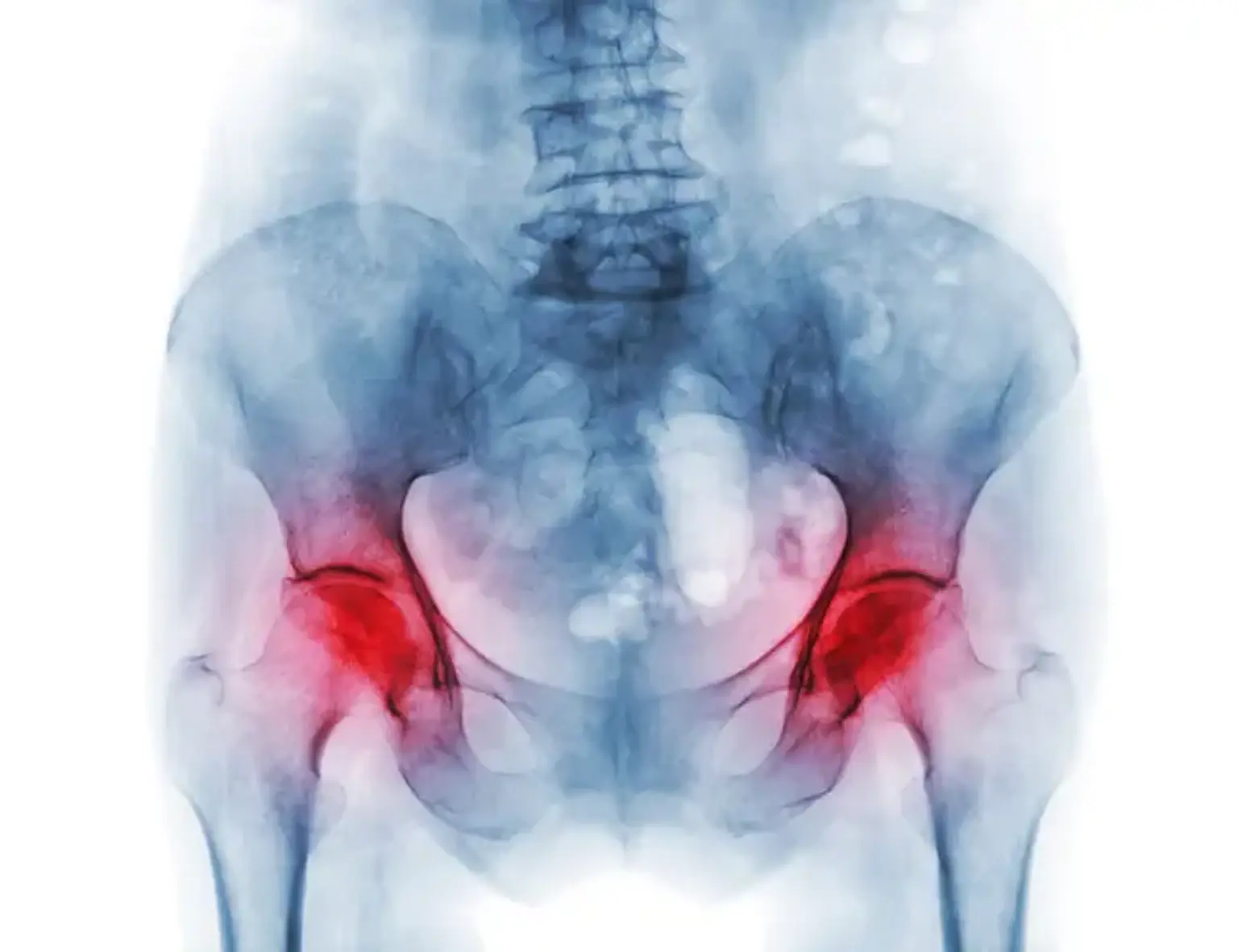
Avascular necrosis (AVN), sometimes called osteonecrosis or bone infarction, is loss of bone tissue due to interruption of the blood supply. There may be no symptoms at first. Joint discomfort may gradually develop, limiting your ability to move. Complications may include bone or joint surface collapse.
Bone fractures, joint dislocations, alcoholism, and the use of high-dose steroids are all risk factors. The condition might sometimes emerge for no obvious cause. The femur is the most usually afflicted bone. Other typical locations are the upper arm bone, knee, shoulder, and ankle. X-rays, CT scans, and MRIs are commonly used to diagnose patients. Biopsies are only utilized in rare cases.
Medication, not walking on the affected limb, stretching, and surgery are all possible treatments. Most of the time surgery is eventually necessary and may include core decompression, osteotomy, bone transplants, or joint replacement. In the United States, around 15,000 cases occur each year. People aged 30 to 50 are the most typically impacted. Males are more likely to be affected than females.