Thoracic aortic aneurysm
Overview
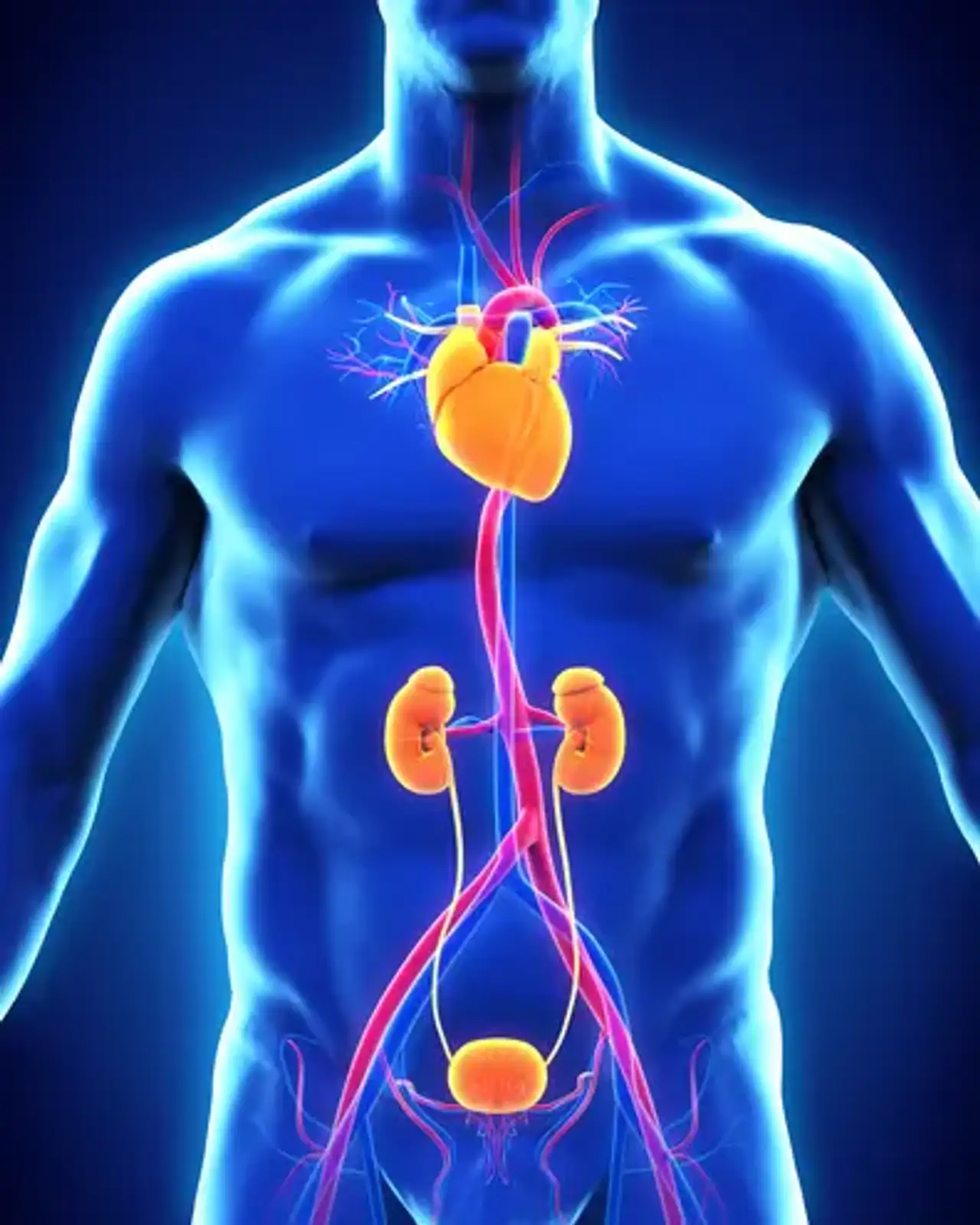
The thoracic aorta is composed of the aortic root, ascending aorta, aortic arch, and descending aorta. An aneurysm arises when the usual diameter of the artery increases by 50%. It happens owing to the aortic wall's inherent fragility. Thoracic aortic aneurysms (TAA) seldom cause symptoms, and around 95% of patients are asymptomatic. These aneurysms, which can cause fatal consequences such as aortic dissection or rupture, are dubbed "silent killers."
What is Thoracic aortic aneurysm?
An aneurysm is defined as a localized or diffuse dilatation of an artery with a diameter that is at least 50% larger than the artery's normal size. Aneurysmal degeneration can occur anywhere in the human aorta; however, the majority of aortic aneurysms (AAs) occur in the abdominal aorta and are hence referred to as abdominal aortic aneurysms (AAAs). A thoracic aortic aneurysm (TAA) is a kind of aneurysmal degeneration that arises in the thoracic aorta.
Thoracoabdominal aneurysms are aneurysms that occur in both segments of the aorta (thoracic and abdominal). TAAs and TAAAs are also susceptible to rupture.
TAAs are subdivided into the following three groups depending on location:
- Ascending aortic aneurysms
- Aortic arch aneurysms
- Descending thoracic aneurysms or thoracoabdominal aneurysms
Aortic aneurysms can extend as far proximally as the aortic annulus and as far distally as the innominate artery, whereas descending thoracic aneurysms begin beyond the left subclavian artery. Arch aneurysms are exactly what their name says.
Another disease that can damage the thoracic aorta is dissection. An intimal rip causes the aortic walls to separate. A fake blood route forms between the layers of the aorta. This false lumen may extend into aortic branches in the chest or belly, resulting in malperfusion, ischemia, or blockage and subsequent consequences. The dissection can also spread proximally, affecting the aortic sinus, aortic valve, and coronary arteries.
Aneurysmal change and early or late rupture can result after dissection. A chronic dissection is one that is discovered more than two weeks after symptoms first appear. Dissection should not be confused with dissecting aneurysm since it can occur with or without aneurysmal aortic enlargement.
An aortic aneurysm can be saccular or fusiform in shape. A fusiform (or real) aneurysm is characterized by a uniform shape and symmetrical dilatation across the full circumference of the aortic wall. A saccular aneurysm is a kind of pseudoaneurysm that is characterized by a localized outpouching of the aortic wall.
Anatomy of the Aorta
A blood vessel has the following three layers:
- Intima (inner layer made of endothelial cells)
- Media (containing muscular elastic fibers)
- Adventitia (outer connective tissue)
Aneurysms might be real or false. A real aneurysm's wall has all three layers, and the aneurysm is confined inside the endothelium. The adventitia contains the wall of a fake or pseudoaneurysm, which only affects the exterior layer. An aortic dissection is caused by an intimal rip and is surrounded by media; therefore, it has a true lumen and a false lumen.
Ascending aortic aneurysms can form as close to the aortic annulus as the innominate artery. They can compress or erode into the sternum and ribs, producing discomfort or creating a fistula. They may also constrict the superior vena cava or the airway. They may include the pericardium, aortic valve, or coronary arteries when symptomatic due to rupture or dissection. They can burst into the pericardium and cause tamponade. They can dissect into the aortic valve and cause aortic insufficiency, or they can dissect into the coronary arteries and cause a myocardial infarction.
Aortic arch aneurysms affect the aorta where the innominate, left carotid, and left subclavian arteries originate. They may obstruct the innominate vein or the airway. They may cause hoarseness by stretching the left recurrent laryngeal nerve.
Descending thoracic aneurysms begin beyond the left subclavian artery and can travel to the belly. According to the Crawford classification, thoracoabdominal aneurysms are classified as follows:
- The descending thoracic aorta from the left subclavian artery down to the abdominal aorta above the renal arteries is involved in Type I.
- Type II extends distally from the left subclavian artery to the renal arteries and may continue to the aortic bifurcation.
- Type III originates in the mid-to-distal descending thoracic aorta and extends as far distal as the aortic bifurcation.
- Type IV originates in the upper abdominal aorta and includes all or none of the infrarenal aorta.
Descending thoracic aneurysms and thoracoabdominal aneurysms can compress or erode the trachea, bronchus, esophagus, vertebral body, and spinal column.
How Common are Thoracic Aneurysms?
Each year, over 13000 persons die in the United States as a result of aortic disease, and TAA is one of the top 18 causes of mortality among all adults. TAA has a case-to-patient-year incidence of 10 and a prevalence of 0.16 to 0.34 percent. TAA is becoming more common as diagnostic imaging improves and life expectancy rises in the general population.
Patients with hereditary TAA present at an average age of 56.8 years, whereas patients with TAA from other sources appear at an average age of 64.3 years. Men are more likely to acquire TAA, but women have poorer clinical results and a higher risk of dissection.
Thoracic Aortic Aneurysm Causes
TAA risk factors include male gender, higher age, a history of hypertension, chronic obstructive pulmonary disease (COPD), coronary artery disease, smoking, and prior aortic dissection. The ligamentum arteriosum is a unique demarcation in the etiology of aortic aneurysms. Above this point, degenerative processes in the elastic media cause aneurysms to develop, whereas atherosclerosis is the culprit below the ligament. This is most likely owing to the different developmental origins of smooth muscle cells in these two locations.
A family history of thoracic aortic aneurysm is a substantial risk factor, as hereditary disorders cause around 20% of TAA cases. Marfan syndrome, Loeys-Deitz syndrome, and Ehlers-Danlos syndrome affect just 5% of persons. Nonsyndromic aneurysms affect around 21% of people with a family history; these aneurysms are known as "nonsyndromic familial aortic aneurysms" and have no extra-aortic signs.
Aortic root dilation is an uncommon complication of left-sided valvular endocarditis. Prior to the discovery of antibiotics, syphilis was the major cause of aortic aneurysms. Takayasu, Behçet, giant cell, Systemic lupus erythematosus, sarcoidosis, rheumatoid arthritis, and ankylosing spondylitis are all types of arthritis that can affect the aorta and cause an aneurysm. Rare causes include a bicuspid aortic valve and an isolated sinus of Valsalva aneurysm. TAA is linked to abdominal aortic aneurysms, cerebral aneurysms, renal cysts, and the bovine aortic arch.
Thoracic Aortic Aneurysms Symptoms
Asymptomatic thoracic aortic aneurysms affect nearly all patients. Patients have the option of reporting chest discomfort. If this discomfort radiates to the back and is accompanied by severe hypotension, it might be an indication of dissection. Compression of neighboring tissues can also cause chest discomfort. Some individuals may exhibit indications of superior vena cava (SVC) syndrome or have trouble breathing owing to airway constriction. Compression of the recurrent laryngeal nerve can cause hoarseness of the voice.
In rare cases, ascending or root aneurysms can cause heart failure owing to rupture in the right atrium or superior vena cava (SVC) or hemoptysis due to lung hemorrhage. Patients should be questioned about any family history of sudden cardiac death. Most aneurysms are silent when examined. A diastolic murmur with expanded pulse pressure might be heard in individuals with aortic regurgitation.
Thoracic Aortic Aneurysm Diagnosis
- CT scan
The most often used imaging approach for diagnosing thoracic aortic aneurysms is a contrast-enhanced CT scan. It is easily accessible and facilitates in the fast assessment of the aneurysm's size, extent, and placement. Calcifications, dissections, and mural thrombus may all be seen clearly. When earlier CT scans are available, compare the present scan to the earliest scan rather than the most recent scan.
- MRI
An axial and 3-D reconstruction of the ascending aorta is provided by MRI. Gadolinium-enhanced MR angiography provides for more precise measurements of the aorta and its branches.
Transthoracic echocardiography (TEE) accurately identifies aortic aneurysms and dissections and is a valid technique for measuring the annulus, sinus, sinotubular junction, and ascending dimensions. TTE is a valid test for checking the aortic root and the degree of aortic regurgitation; however, the distal aorta is not well visible.
- Aortography
During an aneurysm examination, ascending aortography can provide sharp pictures of the aorta contour and lack of the usual "waist" of the sinotubular junction, but size measurements cannot be made.
- PET scans
PET scans are a recent diagnostic tool that can identify regions that "light up," suggesting higher metabolic activity displaying inflammation, signaling impending rupture, and should be used as a preventative measure.
- A chest x-rays
A convex contour of the right superior mediastinum on a chest x-ray may indicate an aortic aneurysm. In the case of an ascending aortic aneurysm, the retrosternal airspace would be absent on the lateral chest x-ray.
- Electrocardiogram (EKG)
The electrocardiogram (EKG) may indicate symptoms of strain and left ventricular enlargement associated with aortic insufficiency. ST elevation or depression might be seen in patients with concurrent coronary artery disease.
TAA may now be detected by genetic testing. Whole-exome and genome sequencing are excellent methods for identifying genes linked to thoracic aortic disease. Patients with high-risk genotypes, such as MYLK, ACTA2, and MYH11 mutations, can be identified quickly.
Thoracic Aortic Aneurysm Management
The goal of medical care is to reduce tension in the aorta, which prevents the aneurysm from growing. Anti-impulse therapy is critical, and beta-blockers are the first-line drugs for stress reduction because they lower blood pressure and contractility. Patients with Marfan syndrome benefit from angiotensin receptor blockers (ARBs) and angiotensin-converting enzyme (ACE) inhibitors because they diminish TGF-B signaling.
Lipid-lowering medications, mostly statins, are also used because they reduce oxidative stress, rupture rate, and dissection. Glucocorticoids, indomethacin, and anti-CD 18 leukocyte-depleting antibodies can also be employed. Fluoroquinolones should be avoided because they worsen wall deterioration in TAA patients. To monitor TAA development in asymptomatic individuals, reimaging should be conducted after 6 months and subsequently yearly if there is no enlargement. To treat hypertension, lifestyle changes such as smoking cessation and food adjustment are recommended.
Surgery
Surgery in TAA patients seeks to avoid aneurysm dissection or rupture. Acute dissection, rupture, or intramural hematoma require rapid surgical repair. When the ascending aorta measures 6 cm and the descending aorta measures 7 cm, the risk of rupture increases. As a result, patients with a 5.5 cm ascending aorta and a 6.5 cm descending aorta should have elective surgery; the cut-off for an ascending aneurysm in an asymptomatic Marfan syndrome patient is 5 cm.
Body size is also considered when planning surgery when the aortic size index (aortic diameter divided by body surface area) is less than 27.5 cm/m. An open surgical technique with aorta replacement is used in TAA of the ascending aorta. The degree of resection is determined by the location of the aneurysmal disease: some patients may be treated well with supracoronary ascending aorta replacement alone, whilst others may require more extensive surgery that may encompass the aortic root or aortic arch.
Replace the sinus segment, ascending aorta, and proximal arch in patients with connective tissue abnormalities, bicuspid aortic valve, or a strong family history of aortic dissection or rupture. At the time of aortic surgery, a bicuspid aortic valve can be replaced or repaired. The median sternotomy, cardiopulmonary bypass, and ischemia arrest with or without deep hypothermic circulatory arrest (DHCA) are all common procedures in open repair.
It is preferable to use DHCA with open distal anastomosis for ascending aorta replacement alone. The aorta is transected 1 cm below the clamp and resected to the sinotubular junction after aortic cross-clamping and cardioplegic arrest. When the target temperature is attained, the cross-clamp is relaxed and a circulatory arrest is triggered. The remaining ascending aorta is removed up to the innominate artery takeoff.
The open aorta is subsequently anastomosed with an adequately sized polyester or polyethylene terephthalate tube graft. Cardiopulmonary bypass is restarted, and a proximal anastomosis to the sinotubular junction is done. Cerebral protective methods, such as antegrade or retrograde perfusion, are available. After the aortic arch has been opened, branched arch grafts or debranching grafts can be employed. Descending TAA can be repaired openly, endovascularly, or with a hybrid treatment.
In open repair, these aneurysms are accessible with a thoracotomy and normally do not require cardiopulmonary bypass or cardioplegia. Thoracic endovascular aortic repair (TEVAR) uses endovascular grafts to repair TAA between the left subclavian and celiac arteries. When the stent edge covers the left subclavian artery, a carotid-subclavian bypass may be done during the surgery. TEVAR takes special precautions to prevent spinal cord ischemia. For elective instances, custom-made branching and fenestrated grafts can be supplied.
Differential Diagnosis
Aortic dissection causes acute ripping chest agony that radiates to the back. Because of increasing stress and aortic wall weakening, it is one of the consequences of TAA. A tear forms in the intima, resulting in the formation of true and false lumens. Patients may also complain of hypotension, nausea, and shortness of breath, as well as a discrepancy in blood pressure between their right and left arms. A broadening of the cardiac silhouette might be noticed on a chest X-ray. The intimal flap and lumens in the aortic wall will be plainly seen on a CT image. The issue must be repaired immediately.
An aortic rupture confined by a thin layer of adventitia is referred to as a thoracic aortic pseudoaneurysm. They form as a result of trauma or the erosion of an atherosclerotic ulcerated plaque. Patients may get chest discomfort or impairment as a result of embolization. This abnormality can be seen with CT scanning and angiography. To avoid aortic rupture, surgical repair is required.
Aortic intramural hematoma is a hematoma that occurs in the aorta's medial layer. Intimal tears are not usually present. They can arise as a result of a penetrating atherosclerotic ulcer or as a result of thrombosis of the false lumen following a dissection. As the hematoma is also a forerunner for aortic dissection, surgical repair is essential to restore the architecture of the aorta wall.
Thoracic Aortic Aneurysm Prognosis
The ascending aortic aneurysm grows approximately 1 mm per year, whereas the descending aortic aneurysm expands by up to 3 mm. When the aorta reaches 6 cm in diameter, its distensibility decreases and it becomes a stiff tube in which increased pressure causes higher stress on the aortic wall. Surgery should be considered for all symptomatic and asymptomatic individuals with a large aneurysm. Patients who have elective surgical correction for TAA have a 5-year survival rate of 85 percent, but those who have emergency surgery have a 5-year survival rate of 37 %.
Complications
An expanding aortic aneurysm can cause aortic dissection and rupture. These problems occur at a comparable rate of 3.5 per 100,000 patient-years. When an ascending aortic aneurysm measures 6 cm in diameter, it has a 34% chance of rupture. Due to high blood pressure levels of up to 300 mmHg, intense emotion and high-intensity weight lifting might cause acute aortic dissection or rupture. Aortic dissection also mirrors circadian and diurnal rhythm patterns, with a greater frequency in the winter and early morning, indicating periods when blood pressure is at its maximum.
Bleeding, stroke, pulmonary dysfunction, cardiac dysfunction, and perioperative death are among surgical consequences. Patients had a perioperative death rate of 28.6 percent with descending aorta surgery and 23.4 percent during endovascular repair. TAA complications of dissection and rupture occurred between 2 and 7.3 percent of the time in an autopsy examination of individuals with sudden cardiac death.
Conclusion
Thoracic aortic aneurysms are a very uncommon condition that has developed in the last few decades as the quality of vascular screening has improved. Several imaging modalities, including thoracic radiography, echocardiography, magnetic resonance imaging (MRI), and positron emission tomography (PET), can be used to diagnose this disease, which is generally diagnosed incidentally.
CTA is the gold standard for aneurysm evaluation because it provides for exact diameter estimation and appropriate preoperative planning. The current European Society for Vascular Surgery recommendations encourage elective treatment of thoracic aneurysms with diameters greater than 55 mm, because dimensions between 55 and 60 mm are linked with a 10% annual rupture risk.
Endovascular repair has been shown to have lower perioperative morbidity and fatality rates than open surgery. According to current standards, the preferred therapy is endovascular, which involves the insertion of an aortic stent graft (thoracic endovascular aortic repair, TEVAR), with open surgery reserved for young patients who are physically suitable for it.